Blastomycosis is a systemic infection caused by inhalation of Blastomyces dermatitidis spores present in soil. B dermatitidis is a dimorphic fungus that grows in the environment as a saprophytic mycelium and is endemic to North America (eg, Mississippi, Missouri, and Ohio River valleys; mid-Atlantic states; southern regions of central and eastern Canadian provinces) but has also been found in Africa and India.1-5 Dogs are most commonly affected as a result of digging and sniffing, but infections have also been reported in cats, ferrets, horses, wolves, captive and noncaptive nondomestic felids, and other wildlife.6-12
Blastomycosis in Companion Animals
Blastomyces dermatitidis in Dogs
Inhalation of B dermatitidis spores results in direct inoculation to the lungs. Spores introduced into the body transform into their yeast form due to body temperature and begin to reproduce asexually. The yeast can then disseminate, resulting in clinical signs (eg, anorexia, fever, weight loss, cough/dyspnea, blepharospasm, miosis, uveitis/blindness, lameness, exudative skin lesions) depending on anatomic location of infection.
Susceptibility to infection is not commonly associated with immune status; however, dogs undergoing immunosuppressive therapy may be at increased risk, and therapeutic modification or discontinuation may help with clinical responses.
Blastomyces dermatitidis in Cats
B dermatitidis infection in cats has only been reported in a few cases; retroviral status is unlikely to serve as an underlying factor. In a retrospective study, FeLV positivity was noted in only 10% of necropsy evaluations of cats with blastomycosis.13 Indoor only cats can acquire systemic infection; therefore, blastomycosis should not be excluded as a differential.14 Clinical course and treatments may parallel those in dogs; however, diagnosis is often made later in the course of disease due to the infrequent prevalence of blastomycosis in cats.
Blastomyces dermatitidis in Ferrets
There is one documented case of blastomycosis in a ferret, which was euthanized due to refractory disease.7 Clinical presentation and signs were similar to those of dogs and cats.
Zoonotic Transmission of Blastomyces dermatitidis
Spread from domestic or nondomestic species to humans can only occur via direct inoculation, as the yeast form does not become airborne or revert to its spore form in the body. B dermatitidis requires physical transmission from one animal to another. Infection following fine-needle aspiration was documented in one clinician,15 and blastomycosis has been reported following dog bites.16 Contact with exudative skin lesions may also result in direct inoculation (although this has not been documented), and care should be taken when in contact with patients with exudative lesions. Overall, human infection is rare, with only a few hundred reported cases.17 Underlying risk factors for severe disease in humans include multilobar lung disease, diabetes mellitus, obesity, and immunosuppression.18
Diagnostics for Blastomyces dermatitidis
Testing is performed in endemic regions whenever infection is suspected. Cytologic evaluation of exudative lesions may confirm diagnosis. Alternatively, fine-needle aspiration and cytology of deeper lesions or lymph nodes, as well as evaluation of bronchoalveolar lavage fluid, can reveal organisms (Figure 1).
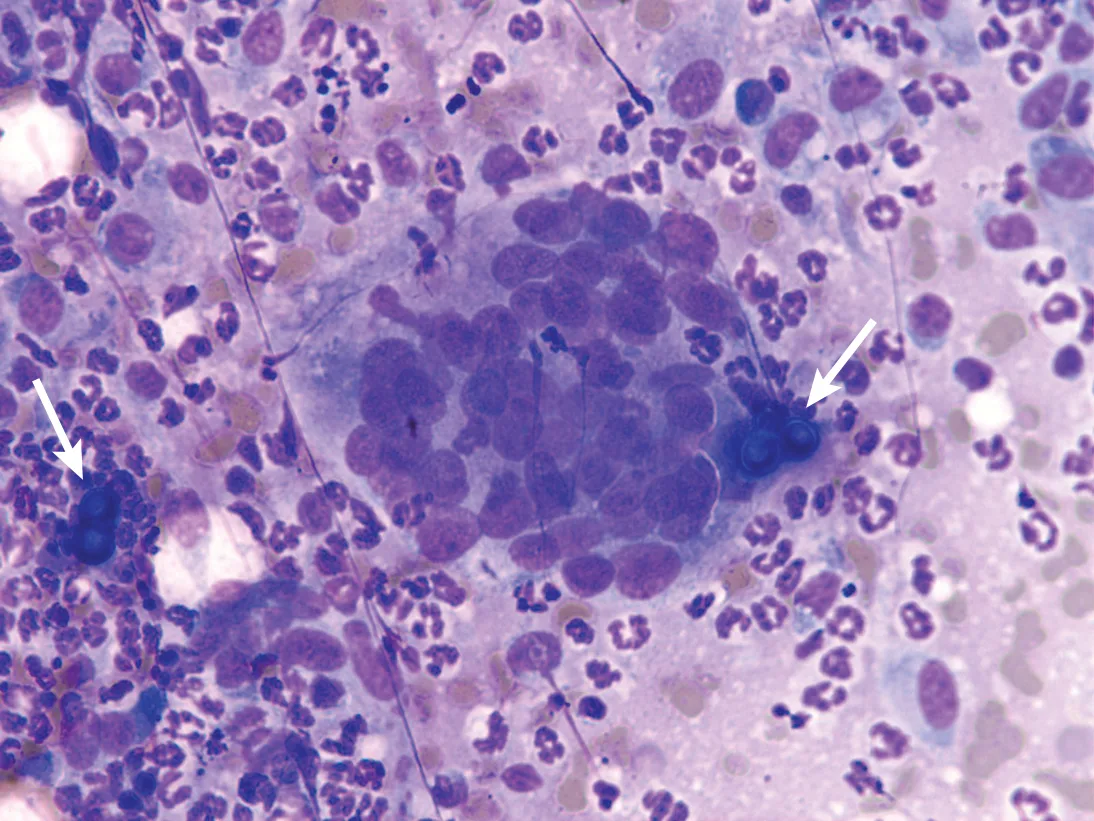
Figure 1 Lymph node aspirate with a pyogranulomatous inflammatory reaction and B dermatitidis yeast (arrows)
Pulmonary changes may include enlarged hilar lymph nodes, alveolar pattern, and either large solitary masses or a diffuse miliary pattern (Figure 2).19 Definitive diagnosis can be made via serum or, preferably, urine evaluated via Blastomyces spp quantitative antigen test.20,21 Biopsy can be performed if suspicion remains despite a negative result. Culture is not routinely performed, as Blastomyces spp culture requires an enhanced biocontainment unavailable in routine diagnostic laboratories.
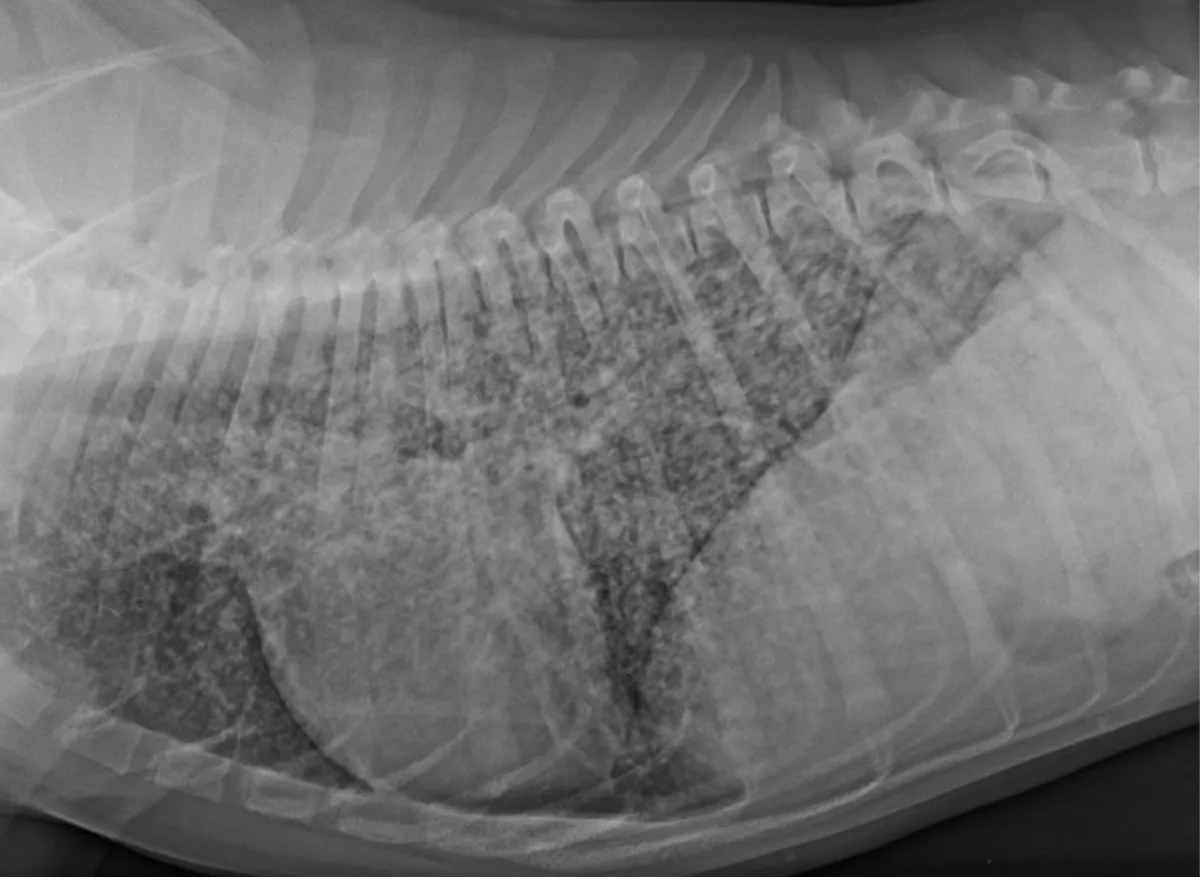
Figure 2 Lateral thoracic radiograph with a diffuse miliary pattern from a 7-month-old, intact male cane corso with a swollen right pelvic second digit, enlarged popliteal lymph node, coughing, and tachypnea
Treatment for Blastomyces dermatitidis
Itraconazole (5-10 mg/kg PO every 24 hours) is the most common treatment for Blastomyces dermatitidis and is often used at the higher dose for ocular infections.22 Compounded formulations have poor absorption and are therefore not recommended despite their cost benefit; however, generic itraconazole has demonstrated equal absorbency with the brand name.23
In patients without ocular or CNS involvement, fluconazole may be as effective as itraconazole after an initial 2-week treatment with itraconazole; however, duration of treatment is likely longer, with a median of 6 months as compared with a median of 4.5 months with itraconazole alone.24 Amphotericin B is often used alone or in combination with an azole in more severe cases (eg, CNS or ocular infection) due to cost and nephrotoxicity associated with amphotericin treatment. Treatment with newer azoles may be considered if standard treatment is ineffective and the patient has pre-existing renal disease.
Efficacy of treatment can be monitored via repeat antigen enzyme immunoassay testing until a zero result is achieved.25 Treatment is often continued for 1 to 3 months after a zero result. A repeat value may be assessed 1 to 2 months after therapy is discontinued to monitor for relapse.
Prognosis
Prognosis is typically favorable. Patients that succumb to disease die or are euthanized within 1 week of diagnosis and treatment.
Vaccination for Blastomyces dermatitidis
No vaccine for B dermatitidis infection is currently available.