
Incidence & Etiology of Canine Aural Hematoma
Aural hematomas are common in dogs, can occur unilaterally (typical) or bilaterally (rare), and are most often caused by trauma (ie, excessive scratching or head shaking) to the pinna that leads to fracture of the auricular cartilage and subsequent hematoma formation between the skin and cartilage of the pinna (Figure 1).1

Aural hematoma involving the left pinna of dog
Underlying causes for excessive head shaking or scratching include otitis externa or media caused by bacteria, yeast, or parasites (eg, mites, fleas); underlying disease processes (eg, atopy, endocrine disease, neoplasia); and hypersensitivity reactions.2-4 An immunologic event that results in degeneration of auricular cartilage is also a possible cause4; however, multiple factors may be present, and the exact pathophysiology has yet to be determined.
Untreated aural hematomas can lead to fibrotic changes that cause thickening and irregular appearance of the pinna (ie, cauliflower ear in humans).
Anatomy of the Canine Ear
The pinna is composed of a thin layer of auricular cartilage covered by hairless skin on the concave side and haired skin on the convex side. Blood supply to the skin and cartilage arises from the auricular arteries and veins that run longitudinally on the medial (cranial or rostral) and lateral (caudal) margins of the pinna (Figure 2).
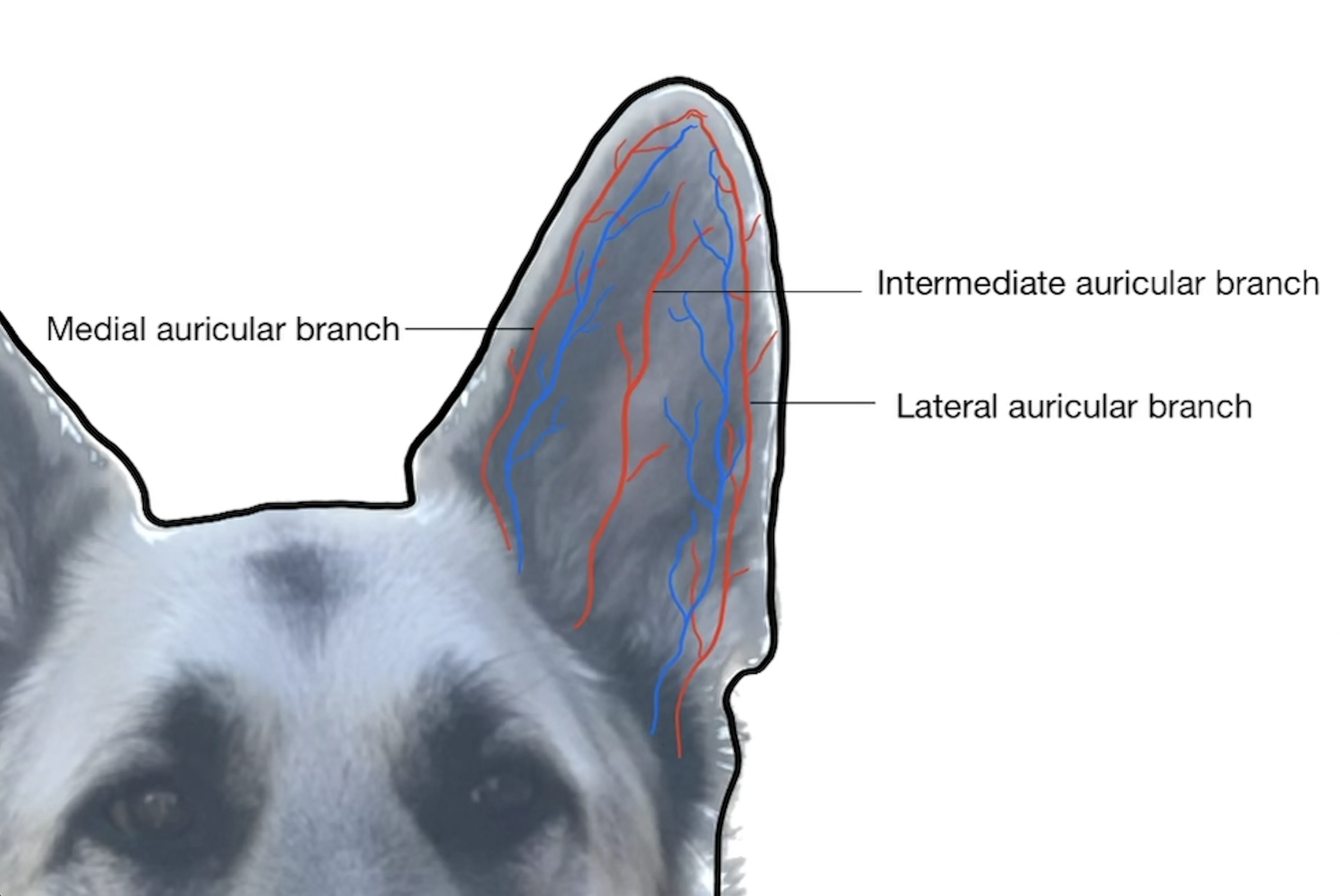
Illustration of the vascular supply to the pinna of a dog. Vessels run predominantly on the medial (cranial or rostral) and lateral (caudal) margins of the pinna.
Treatment of Aural Hematoma in Dogs
Accurately diagnosing and treating the underlying cause of excessive head shaking or scratching is a core component of overall management.
Treatment approaches include surgical management, less-invasive management with active or passive drainage, and conservative management (ie, aspiration and local corticosteroid injection, oral corticosteroid therapy alone). With the exception of oral corticosteroid therapy alone, treatment goals should be to remove hematoma contents, provide continuous or intermittent drainage, and allow for reapposition of the layers of the pinna to reduce the risk for recurrence. Treatment should be based on the patient’s comorbidities or risks associated with general anesthesia, cost, patient and pet owner compliance, and clinician preference and experience.
Surgical Management
Surgical management typically results in a positive outcome and minimal recurrence.5 Surgery involves incising the skin over the hematoma to allow drainage and flushing, then directly reapposing the pinna layers with sutures.
Less-Invasive Management
Passive and active drains are less-invasive options for managing aural hematomas and typically do not require general anesthesia6-8; however, risk for reaccumulation of fluid after drain removal and delayed healing may be increased because the pinna layers are not directly apposed.
Passive Drains
Passive drains (eg, teat cannulas) should be placed into the hematoma on either the concave or convex side of the distal aspect of the pinna (Figure 3). The drain should be placed via a small stab incision and secured to the skin with a purse-string or other type of securing suture. After the hematoma is drained, the pinna should be bandaged over the head to provide compression and promote adhesion of the skin and cartilage. Disadvantages of passive drains include more frequent bandage changes depending on the volume of fluid produced and risk for ascending infection via the drain site. Similar to other wound drains, the drain should be removed once fluid production has decreased and reaccumulation is less likely (≈7-10 days).

Teat cannula placed at the tip of the pinna for continuous hematoma drainage
Active Drains
Active or closed-suction drains use negative pressure from a collection chamber to maintain continuous drainage, collapsing the dead space created by the hematoma and bringing the pinnal layers together to promote adhesion and healing. Advantages of active drainage include the ability to quantify fluid production and potential reduced risk for ascending infection due to the closed nature of the system; however, maintaining placement of the tubing and suction unit can be difficult, and occlusion of the drain tubing can lead to loss of suction.
Conservative Management
Conservative management involves aspiration of the hematoma followed by local injection of corticosteroids (eg, triamcinolone, dexamethasone) into the existing dead space. Alternatively, administration of oral corticosteroids (eg, prednisolone) alone (without aspiration or other drainage) has been described as a conservative option.9-11 Corticosteroids reduce inflammation within the pinna, thus decreasing fluid production responsible for separating the skin from the cartilage.
Repeated aspiration is typically required because of ongoing fluid production; however, one study reported clinical improvement (ie, subjective improvement in pinna status) in 87.5% of dogs treated with oral prednisolone alone.11
The primary disadvantage of a less-invasive or conservative approach is lack of direct apposition of the pinna layers, which may increase the risk for reaccumulation of fluid and delayed healing.
Potential Complications of Canine Aural Hematoma Treatment
Potential complications of treatment include recurrence, infection, cellulitis, and thickening or scarring of the pinna; however, these can be avoided or reduced with early management, careful tissue handling, and bandaging of the ear to provide gentle compression and prevent shaking and trauma to the pinna.
Clinical Skills You’ll Want to Keep
Get this guide in a free downloadable resource, along with guides to 5 more cornerstone skills you'll want to have in your back pocket. From choosing the correct fluid type to performing a neurological examination, Practical Guidance for New Veterinarians is your key to starting practice with confidence.
Step-by-Step: Surgical Treatment for Canine Aural Hematoma
What You Will Need
Cotton ball or gauze
Electric clippers
Surgical scrub (eg, chlorhexidine scrub)
Sterile surgical drapes
Sterile gloves
#15 scalpel blade
Scalpel blade handle
Sterile saline flush and device for flushing (eg, syringe, catheter, needle)
Needle drivers
Absorbable or nonabsorbable suture material
Mayo scissors
Bandage material (eg, cast padding, absorbent stretch conforming gauze, self-adherent bandages)
Alternatives: elastic stockinette, custom-sized head wrap
Elizabethan collar
Step 1: Prepare the Patient
Anesthetize and place the patient in lateral recumbency with the affected ear exposed. Insert a cotton ball or gauze into the ear canal to help prevent surgical scrub, flush, and hematoma contents from entering the canal. Clip hair from both sides of the affected pinna, scrub the area with surgical scrub, and drape the site using sterile surgical drapes. If indicated, collect a sample of fluid via fine-needle aspiration for cytologic examination.

Step 2: Make an Incision
Using a #15 scalpel blade, make a longitudinal or S-shaped incision over the hematoma on the concave aspect of the pinna. Only extend the incision through the skin to allow draining and flushing. Do not extend the incision through the auricular cartilage.

Author Insight
An S-shaped incision may reduce the likelihood of cosmetic deformities caused by longitudinal contracture of the incision. Alternatively, a dermal punch or carbon dioxide laser can be used to create defects in the skin on the concave side of the pinna for hematoma drainage.12 Use of a carbon dioxide laser may create adhesions between the skin and underlying cartilage acting as an alternative to suture placement; however, suturing the S-shaped incision is often preferred, as this provides a direct and more secure apposition of the skin to the auricular cartilage. The number of sutures should be based on clinician preference and provide adequate reduction of dead space.
Step 3: Flush with Sterile Saline
Once the hematoma has been drained, flush any remaining fluid or clots using sterile saline.
Step 4: Place Sutures
Using nonabsorbable, monofilament suture material (eg, 3-0 or 4-0 nylon), place sutures ≈8 to 10 mm apart using either a partial- or full-thickness mattress pattern. Keep the skin incision slightly open for continued drainage and healing by second intention.

Author Insight
Mattress sutures should be placed parallel to the long axis of the pinna to minimize incorporation of the auricular vasculature, as this could result in avascular necrosis of the pinna. Any suture pattern can cause avascular necrosis if accidental ligation of the auricular vasculature occurs.
In patients with an excessively swollen pinna or anticipated progressive swelling, stenting the mattress sutures may minimize the risk for sutures becoming embedded in the skin and causing additional irritation. Stents can be fashioned from latex tubing or other soft material (A). Despite the use of stents, some scarring on the concave aspect of the pinna may occur (B).

As an alternative to full-thickness sutures, intradermal sutures may be used to minimize the reaction to external sutures and eliminate the need for suture removal.13 Using a simple continuous pattern, a row of sutures (ie, 4-0 synthetic absorbable material) can be placed through the dermis on the underside of the skin and the superficial surface of the cartilage on each side of the incision to provide apposition of the tissue layers.
Step 5: Bandage the Pinna
Bandage the pinna and head, and fit an Elizabethan collar prior to recovery from anesthesia.
Author Insight
Bandaging the pinna for 1 to 2 weeks after drainage can minimize further trauma from continued head shaking and reduce the risk for incision or suture infection during healing. Maintaining bandage position and preventing slippage can be difficult in some dogs. Traditional bandaging techniques use cast padding, absorbent stretch conforming gauze, and self-adherent bandage materials to encompass both the head and affected pinna. Alternatively, an elastic stockinette or custom-sized head wrap can be used, as these are generally easier to replace and allow convenient evaluation of the sutures or drain. Modifications may allow the unaffected pinna to exit freely from the stockinette or bandaging, reducing the occurrence of bandage slippage.

Monitoring bandages for excessive tightness or slippage is critical because of increased risk for compression of the airway and asphyxiation.
An Elizabethan collar should be used whether or not a bandage is present to prevent self-trauma of the pinna and to protect the incision or drain.
Step 6: Remove the Sutures
Remove the sutures after 2 to 3 weeks if the incision has healed and the layers of the pinna are well apposed. Allow any remaining gaps in the incision to heal by second intention, noting the risk for recurrence if the layers are not well apposed and fluid reaccumulates in the pinna.
Author Insight
Continued monitoring for recurrence and incisional healing is recommended.