Case Studies: Understanding Canine Addison’s Disease
J. Catharine Scott-Moncrieff, MA, MS, Vet MB, DACVIM, DECVIM, Purdue University

Clinical signs
Hypoadrenocorticism (Addison’s disease) results from failure of the adrenal glands to secrete glucocorticoids and mineralocorticoids. Most cases are due to primary adrenal failure, resulting in deficiency of usually both cortisol and aldosterone secretion from the adrenal cortex. Clinical signs may be vague, can wax and wane and include anorexia, vomiting, lethargy, depression, weakness, weight loss, diarrhea, shaking/shivering, polyuria, polydipsia, bradycardia, weak pulse and collapse. Owners may not realize how long their dog has been ill until treatment results in a dramatic improvement in activity level.
Laboratory abnormalities
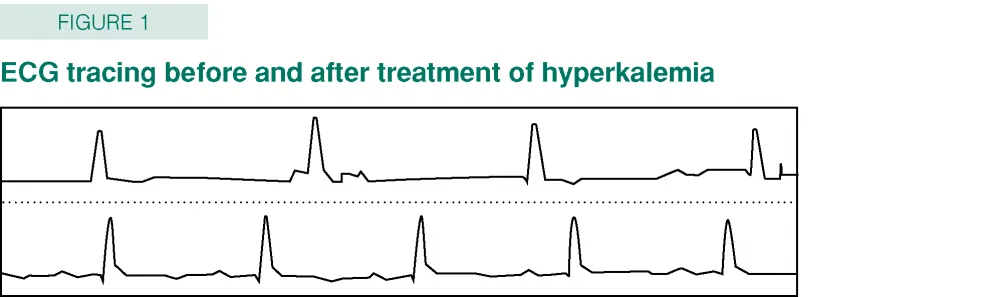
Abnormalities on a complete blood count (CBC) may include anemia, eosinophilia, neutrophilia and lymphocytosis. Hemoconcentration and lack of a stress leukogram may also be present. A chemistry profile may reveal hyponatremia, hypochloremia, hyperkalemia, hypercalcemia and hyperphosphatemia. Not all dogs with hypoadrenocorticism have the expected electrolyte changes. Other biochemical abnormalities may include hypoalbuminemia, hypocholesterolemia, hypoglycemia and increased liver enzymes. Specific gravity of the urine is commonly less than 1.030. In dogs with hyperkalemia, abnormalities may be present on the electrocardiogram (ECG). These include a peaked T wave and shortening of the QT interval in mild hyperkalemia, widening of the QRS complex, decreased QRS amplitude, increased duration of the P wave, and increased P-R interval in moderate hyperkalemia, and loss of P waves and ventricular fibrillation or asystole in severe hyperkalemia. Many other disorders may mimic the characteristic findings of Addison’s disease.
ACTH stimulation test
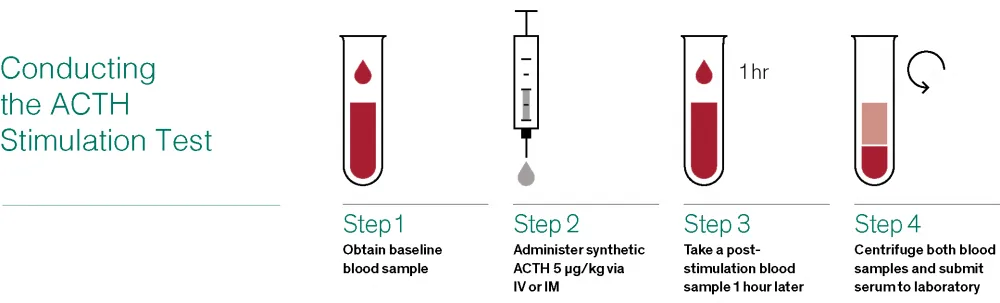
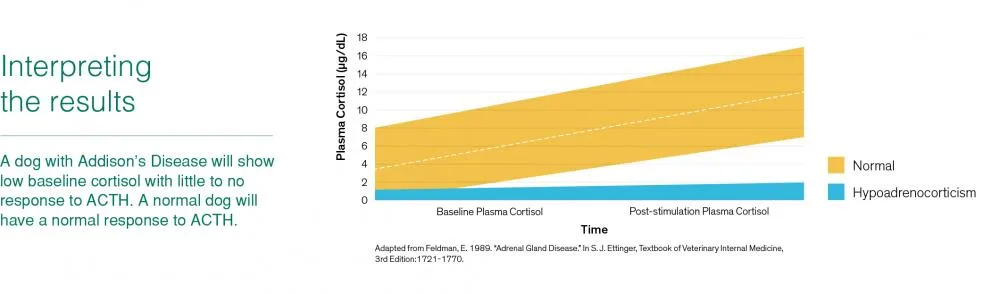
An ACTH (adrenocorticotropic hormone) stimulation test is necessary to confirm a diagnosis. Blood samples to measure serum cortisol levels should be collected prior to and one hour after injection of a synthetic form of ACTH (up to 5 µg/kg). To confirm the diagnosis both the pre- and post-ACTH cortisol concentrations should be less than the reference range for basal cortisol (2 μg/kg). Measurement of a basal cortisol of >2 μg/kg is a useful test to exclude a diagnosis of hypoadrenocorticism.
Treatment
Rapid initiation of treatment of confirmed Addison’s disease is vital, especially if profound electrolyte abnormalities are present. Aims of treatment include correction of hypotension/hypovolemia, correction of electrolyte imbalances, provision of an immediate source of glucocorticoids, and correction of acidosis, hypoglycemia and hypercalcemia. Parameters that should be monitored during treatment include serum electrolytes and acid-base status, urine output, ECG and blood pressure. Fluid therapy and IV glucocorticoids should be continued until the animal is fully rehydrated and oral intake is possible.
The most appropriate treatment for long-term mineralocorticoid replacement is desoxycorticosterone pivalate (DOCP) at a starting dose of 2.2 mg/kg (1 mg/lb) every 25 days. The dose should be titrated to effect. In many cases the final individualized dose of DOCP is < 2.2 mg/kg. Prednisone is recommended for glucocorticoid replacement. The starting dose is 0.2 mg/kg per day and the dose should be tapered to the lowest dose that will control the clinical signs. It is important to avoid excess prednisone supplementation because this may result in manifestations of iatrogenic hyperadrenocorticism.
Case studies
The following case studies provide examples of the variable clinical signs of canine hypoadrenocorticism and the value of early diagnosis and prompt initiation of treatment with Percorten®-V (desoxycorticosterone pivalate injectable suspension). Percorten-V is indicated for the treatment of canine Addison’s Disease.*
*For use as a replacement therapy for the mineralocorticoid deficit in dogs with primary adrenocortical insufficiency.
Important Safety Information
Case in Brief
Diagnosis and Treatment of Canine Addison’s Disease
Signalment
9-year-old Male Neutered West Highland White Terrier
History
Owner reports an 8-month history of mild intermittent diarrhea that has become worse in the last two weeks. During this time the color of the feces has become very dark. The dog was receiving no medications apart from routine heartworm prophylaxis and sucralfate, which had been prescribed for suspected melena. The dog was last vaccinated ten months ago.
Physical examination
The dog was quiet but alert. Body temperature was normal at 101.5°F, heart rate was 80 beats per minute and respiratory rate was 20 breaths per minute. Body weight was 8.5 kg and body condition score was 4/9.
Diagnostic plan
Blood was collected for a CBC, serum chemistry profile and urinalysis. Abnormalities included hypoproteinemia, non-regenerative anemia, hypocholesterolemia and hypocalcemia (see tables 1 and 2). The urinalysis had a specific gravity of 1.025, with negative protein and a benign sediment.
Complete Blood Count Results
Selected Values From Chemistry Panel
Anisocytosis 1+, Poikilocytosis 1+ Polychromasia noted, reactive lymphocytes noted.
Further diagnostic testing
Pre- and post-feeding bile acids were within the reference range. An ACTH stimulation test showed both a pre- and post-cortisol of < 1 µg/dl which was diagnostic for hypoadrenocorticism (Addison’s disease). Endogenous ACTH concentration was elevated (813 pg/ml reference range 10-40) consistent with primary Addison’s disease.
Initial treatment plan
Initial treatment was with prednisone 0.22 mg/kg PO q 24 hours. This dose was tapered to 0.1 mg/kg q 24 hours over the following month.
Monitoring and outcome
The dog was monitored carefully for signs of mineralocorticoid deficiency (polyuria, polydipsia, weakness, depression, bradycardia), and electrolytes were monitored monthly for the first three months and then every three months. Eight months later development of hyperkalemia and hyponatremia prompted treatment with Percorten-V (desoxycorticosterone pivalate injectable suspension) (2.2 mg/kg or 1 mg/lb IM q 25 days).
Key point
Veterinarian’s comments
This case is a good example of atypical canine Addison’s disease. If an ACTH stimulation test had not been performed in this dog, the Addison’s disease would have been missed and the dog would have likely undergone an unnecessary gastroduodenoscopy procedure. Clues that this dog had Addison’s disease included the non-specific gastrointestinal signs, lack of a stress leukogram, and presence of non-regenerative anemia, hypocholesterolemia and hypoalbuminemia. It is important for clinicians to appreciate that dogs with Addison’s disease can present with a wide variety of clinical signs. Affected dogs may have marked hypoalbuminemia and hypocholesteremia and present with clinical signs that are similar to other causes of protein-losing enteropathy in dogs such as inflammatory bowel disease, lymphangiectasia and lymphoma. Dogs diagnosed with atypical Addison’s disease should be carefully monitored because they may have progression of their disease and develop electrolyte abnormalities. This usually happens within 12 months of the diagnosis of primary hypoadrenocorticism.
See important safety information above.
Case in Brief
Diagnosis and Treatment of Canine Addison’s Disease
Signalment
18-month-old Female Spayed Irish Terrier

History
Owner reports a 2-day history of decreased activity, depression and anorexia. A similar episode two months previously resolved with supportive care. The dog has not received any medications and was last vaccinated six months ago.
Physical examination
The dog was laterally recumbent and lethargic. Mucous membranes were injected, hyperemic, and tacky. Capillary refill time was prolonged at three seconds. Body temperature was low at 95.1°F, the dog was bradycardic, with heart rate and pulse of 48 beats per minute. Respiratory rate was normal (16 breaths per minute). Body weight was 16 kg and body condition score was 5/9. Blood pressure was too low to measure.
Complete Blood Count Results
Selected Values From Chemistry Panel
Diagnostic plan
Blood was collected and an ACTH stimulation test performed. The bladder was too small to collect urine. Blood abnormalities (CBC, serum chemistry panel) included hemoconcentration, severe hyperkalemia (10.5 mmol/l), hyponatremia (128 mmol/l), and azotemia (BUN 201 mg/dl, creatinine 6.9 mg/dl) (see tables 3 and 4). An ECG showed atrial standstill. P waves were absent and the duration of the QRS complex and QT interval were prolonged (see figure 1).
Initial treatment plan
Initial treatment for the hypovolemic shock and hyperkalemia included IV catheter placement and fluid resuscitation with an IV saline bolus followed by a saline infusion (6 ml/kg/hour). Drugs administered included dextrose, insulin, calcium gluconate and bicarbonate to decrease the serum potassium concentration and protect the myocardium from the effects of hyperkalemia. The arrhythmia resolved and the heart rate normalized. Because of the clinical diagnosis of Addison’s disease, the dog was also treated with IV dexamethasone (initial dose 0.2 mg/kg then 0.1 mg/kg in IV fluids), and one dose of Percorten-V (desoxycorticosterone pivalate injectable suspension) (2.2 mg/kg or 1 mg/lb IM).
Outcome
The ACTH stimulation test showed both a pre- and post-cortisol of < 1 µg/dl confirming the diagnosis of hypoadrenocorticism (Addison’s disease). The dog responded well to treatment and was discharged on prednisone at a dose of 0.25 mg/kg PO q 24 hours with plans to taper the dose over the next few weeks to 0.1 mg/kg of prednisone or less. The dog was scheduled for a recheck visit in two weeks and follow up Percorten injection 25 days from presentation.
Key point
Veterinarian’s comments
This case is a good example of the appropriate management of an acute presentation of Addison’s disease. A delay in treatment would have resulted in death due to hyperkalemia. The severe bradycardia in the presence of hypovolemic shock suggested hyperkalemia even before laboratory results were available. In patients with severe hyperkalemia, strategies to rapidly decrease the potassium concentration (administration of dextrose, insulin and sodium bicarbonate) and to protect the myocardium (calcium gluconate) are needed. The history that included a previous less severe episode was typical for dogs with Addison’s disease. Because Addison’s disease was diagnosed on the history and the acute clinical presentation, Percorten-V (DOCP) was administered prior to receiving laboratory results. Other abnormalities that supported the diagnosis included azotemia and lack of a stress leukogram.
See important safety information above.
Percorten, Elanco and the diagonal bar logo are trademarks of Eli Lilly and Company or its affiliates.
© 2017 Eli Lilly and Company or its affiliates. USCACPER00025
