Diagnosing Canine Exophthalmos
Jessica McDonald, DVM, Eye Care for Animals, Salt Lake City, Utah
Amy Knollinger, DVM, DACVO, Eye Care for Animals, Salt Lake City, Utah

You have asked...
What is the best way to diagnose and treat exophthalmos in dogs?
The experts say...
Diseases in the orbit are uncommon and typically produce clinical signs by changing the volume and/or function of the orbital structures. In the early stages of orbital disease, clinical signs are generally nonspecific and may include mild prolapse of the third eyelid, periorbital swelling, temporomandibular pain, anisocoria, blindness, exophthalmos (protrusion of the eyeball), enophthalmos (posterior displacement of the eyeball), or deviation of the globe (strabismus; Figure 1).1,2

Left eye of a 14-year-old dog with unilateral exophthalmos. Note the third eyelid protrusion, dorsolateral deviation of the globe, ventral deviation of the third eyelid, and epiphora in the medial canthus.

Image of retropulsion performed on a dog. The upper eyelid is closed and the globe is pushed into the orbit. This can be performed in both eyes simultaneously to determine if there is any difference in retropulsion between the eyes.
Exophthalmos should be differentiated from buphthalmos (increased size of the globe) resulting from a chronic increase in intraocular pressure or glaucoma.1-3 Retropulsion can help discern the compressibility of the orbital contents, which is limited with a space-occupying lesion. This is performed by closing the eyelids over the globe and pushing the globe into the orbit (Figure 2). If a space-occupying lesion is present, globe displacement within the orbit may vary depending on the location. Space-occupying lesions within the extraocular muscle cone generally push the globe straight forward, whereas lesions outside the extraocular muscle cone push the globe opposite the location of the lesion.2 The onset of clinical signs can also help determine the cause of orbital disease. Acute onset is more consistent with inflammatory disease; slower onset is more suggestive of a neoplastic process, mucocele, or cyst.2
Read more: Differentiating Exophthalmos, Buphthalmos, & Proptosis
Related: Exophthalmos in a Dog
Retropulsion can help discern the compressibility of the orbital contents, which is limited with a space-occupying lesion.
Orbital Disease Diagnostics
Many diagnostic tests and procedures can be performed to evaluate orbital disease. A general physical examination is helpful for diagnosing orbital disease. Apparent pain when palpating around the periorbital region as well as pain on opening the mouth (as a result of compression of the abnormal orbital contents by the ramus of the mandible) can be indicative of orbital disease. Pain is most consistent with an inflammatory process but can also be present if an advanced neoplasia is present. Although skull radiography is often low-yield and nonspecific, it can be used to detect involvement of the adjacent nasal cavity, sinuses, or tooth roots. Ultrasonography can be used to identify orbital lesions for guided biopsy but is also often low-yield. Advanced imaging procedures (eg, MRI, CT) have become the gold standard for orbital imaging. Like ultrasonography, CT can be used to guide biopsy and provide a definitive diagnosis. These modalities can identify foreign bodies, locate lesions, and define the extent of disease. This can be used for diagnostic and treatment planning as well as prognosis.4
Common Causes of Orbital Disease
Diagnostic differentials for orbital disease can be extensive, and a thorough workup is needed before treatment can begin. This article focuses on the more common causes; Other Causes of Orbital Disease in Dogs lists additional causes.
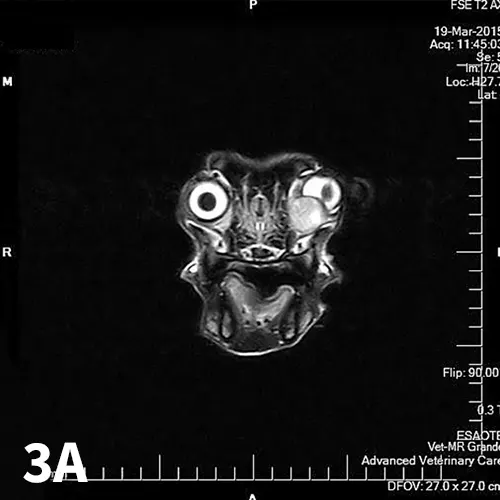
(A) Axial T2-weighted and (B) sagittal T2-weighted postcontrast MRI images of the dog in Figure 1 with a mixed orbital carcinoma. Note the lobular mass ventromedial to the left eye. It is causing dorsolateral distortion of the ventral globe.
Orbital Neoplasia
Orbital neoplasia (Figure 3) can be classified as primary (involving the orbital tissue directly) or secondary (arising from a distant site or extension of a contiguous structure). Approximately 90% to 95% of all orbital neoplasias are malignant in the dog and cat,2 with 92% and 58% being primary in the dog and cat, respectively.5 Orbital neoplasias are usually associated with slowly progressive exophthalmos and minimal pain, although approximately one-third of orbital neoplasias are painful.2 MRI or CT is used to localize and define the margin of orbital tumors. Usually, excision of these tumors is not curative. Orbital exenteration—removal of all orbital contents, including the globe—is advised, even in a visual eye. Consultation with a veterinary oncologist for potential chemotherapy or radiation therapy is strongly recommended owing to the aggressive, malignant nature of these tumors.1-3,5
Orbital Abscess
Retrobulbar abscesses causing acute, moderate-to-severe exophthalmos are typically painful. Treating an orbital abscess empirically with an extended course of medications for at least 4 weeks may be sufficient, especially early in the course of disease. Antibiotics (against both aerobic and anaerobic organisms), NSAIDs, and pain medications should be used. Oral corticosteroids should be avoided if in doubt about the presence or absence of infection. A topical lubricant is indicated if lagophthalmos (inability to perform a complete blink response) is present. If lagophthalmos is severe, a temporary tarsorraphy should be performed. Topical corticosteroid medications are contraindicated because of the increased risk for corneal ulceration caused by corneal exposure. Lubricants without an antibiotic are indicated if no evidence of ocular surface infection or corneal ulceration is present.
Recurrence after stopping medical therapy may require surgical exploration or referral to a veterinary ophthalmologist. Abscesses can be drained under general anesthesia. The oral mucosa behind the last upper molar tooth is often swollen and inflamed. The mucosa is incised and closed hemostats are introduced into the orbit through the incision. The hemostats are opened and withdrawn without closing to establish drainage of the abscess. If no improvement is noted or the globe is blind, enucleation or exenteration can be considered for comfort purposes.
Orbital Cellulitis
Orbital cellulitis, or inflammation within the orbit, is typically acute and may be misinterpreted as conjunctivitis in early stages. Retropulsion is decreased, and there can be significant pain on opening the mouth. Extension of inflammation from a tooth root, nasal sinus, or zygomatic salivary gland can cause orbital cellulitis, as can inflammation from migrating or penetrating foreign bodies. Depending on the cause of infection and the severity of exophthalmos, medical therapy alone, including empiric antibiotics and anti-inflammatory medications for a minimum of 4 weeks, may be adequate treatment. Blindly draining any inflammatory process via the mouth is not advised, as excessive damage to the optic nerve and associated orbital structures can occur with minimal-to-no drainage.
Related Article: Top 5 Dental Emergencies
Related Article: The Case: Retrobulbar Abscess or Something Else?
Orbital Mucocele
Orbital retention cysts or mucoceles may arise from the zygomatic salivary gland, lacrimal glands, conjunctiva, or paranasal sinus mucosa. The typical presentation is nonpainful exophthalmos accompanied by a prominent third eyelid. A fluctuant conjunctival swelling may be found on ocular examination, or swelling of the zygomatic salivary duct or the mucosa behind the last upper molar may be found on oral examination. Typically, orbital mucoceles and retention cysts require surgical excision; however, successful use of intracystic polidocanol has also been reported.6
Orbital disease is a rare, potentially devastating disease of the dog that can present in many different ways, especially in early disease process. Imaging with routine modalities can be difficult, therefore advanced imaging (eg, MRI, CT) is highly recommended for diagnosis if clinical signs are observed.
OTHER CAUSES OF ORBITAL DISEASE IN DOGS1
Orbital neoplasia: primary or secondary
Retro-orbital neoplasia: bone, sinuses, nasal and oral cavity
Orbital abscess
Orbital cellulitis
Retro-orbital cellulitis/abscess: tooth root, zygomatic sialadenitis, foreign body, fungal granuloma
Orbital mucocele: zygomatic origin
Orbital cysts
Orbital hemorrhage: trauma, blood dyscrasia, clotting deficiencies
Arteriovenous fistula
Myositis of ocular muscles
Myositis of muscles of mastication
Mandibular hypertrophic osteoarthropathy