
Fluid therapy is essential for common conditions (eg, dehydration, hypovolemia, electrolyte abnormalities, acid–base disturbance) in cats and dogs and can be the cornerstone of therapeutic management in critically ill patients.1,2 Formulation of a fluid therapy plan requires knowledge of fluid types, specific fluid compositions, therapeutic recommendations, and possible iatrogenic adverse effects.3 This article discusses how to choose the most appropriate fluid type and calculate fluid rates in dogs and cats. Additional information (eg, fluid therapy for anesthesia, electrolyte supplementation, acid–base disorders, outpatient fluid therapy) is available elsewhere in the literature.2-11
It is estimated that ≈60% of a cat’s or dog’s body weight is comprised of water (total body water). Total body water is distributed in the intracellular, interstitial, and intravascular (plasma) spaces. Fluid losses from these spaces occur due to various clinical diseases, and fluid therapy aims to restore fluid balance (Figure).
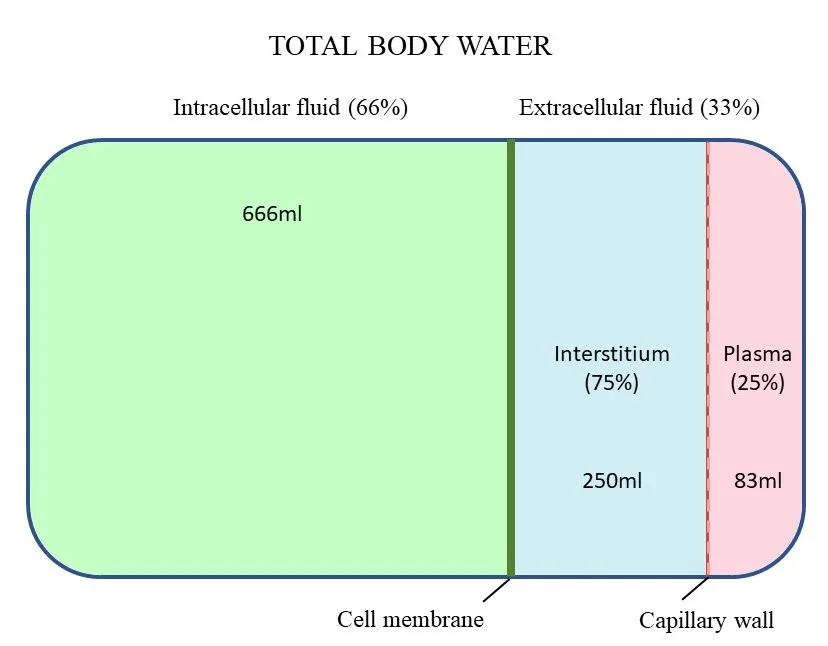
Volume of water in each body compartment, considering a patient with a total body water of 1,000 mL (values are approximate). Not represented is a small amount of fluid in the transcellular space (eg, cerebrospinal fluid, joints).
Crystalloids & Colloids
Fluids are divided into crystalloids and colloids. Crystalloids are solutions that contain electrolytes and other small, water-soluble molecules and/or dextrose. Crystalloids may also contain buffers (eg, lactate, gluconate, acetate) typically converted to bicarbonate or a bicarbonate precursor to maintain the body’s acid–base status and are generally categorized as isotonic (Table 1), hypotonic (Table 2), or hypertonic based on tonicity relative to plasma. Moreover, crystalloids vary in their concentration of electrolytes.12 Colloids are fluid types that contain macromolecules suspended in a crystalloid solution and are used to support intravascular volume or raise plasma oncotic pressure. Colloids are not discussed in detail in this article, but additional information is available.12,13
Table 1: Isotonic Crystalloids
aBalanced solutions (ie, bicarbonate is produced as final product of lactate, acetate, and/or gluconate metabolism)
bNormal blood osmolality: dogs, 290 to 310 mOsm/L; cats, 311 to 322 mOsm/L
Table 2: Hypotonic Crystalloids
aBalanced solutions (ie, bicarbonate is produced as final product of acetate metabolism)
bMay be classified as an isotonic or hypotonic solution; initially isotonic, but becomes hypotonic when dextrose is metabolized
cNormal blood osmolality: dogs, 290 to 310 mOsm/L; cats, 311 to 322 mOsm/L
dThese solutions have lower sodium concentration compared with normal serum sodium concentration (140-155 mEq/L) in dogs and cats.
Choosing the Right Fluid Therapy Plan
It is important to first identify whether the fluid deficit is in the interstitial or intravascular space. Significant fluid deficit in the intracellular space (manifesting as hypernatremia) occurs less commonly than in the extracellular space and is not discussed in this article.
Dehydration
Fluid deficit in the interstitial space is dehydration and manifests as dry mucous membranes, skin tenting, sunken eyes, doughy abdomen, and dry corneas. Dehydration may also be characterized by elevated hematocrit, total protein/solids, BUN, serum creatinine, and/or urine specific gravity. Most clinical patients with dehydration are usually 5% to 8% dehydrated; more profound dehydration can occur but is uncommon. Vomiting and diarrhea are the most common causes of fluid loss, inducing dehydration.
Hypovolemia
Fluid deficit in the intravascular space is hypovolemia, caused either by severe isotonic fluid loss or hemorrhage, and manifests as tachycardia, weak peripheral pulses, pale mucous membranes, altered mentation, prolonged capillary refill time, and cold extremities. Hyperlactatemia (lactate, ≥22.5 mg/dL [2.5 mmol/L]) and hypotension may also be identified. Cats with hypovolemia have a classic triad of hypotension, bradycardia, and hypothermia.
IV Fluid Options
Isotonic crystalloids are the fluid type of choice for treating dehydration. When multiple isotonic fluid options are available, an isotonic crystalloid fluid type that aligns most closely with the patient’s sodium concentration may be selected.
In humans, high-chloride fluids (eg, 0.9% sodium chloride) may be associated with increased risk for acute kidney injury (AKI) and mortality.14,15 In dogs, the relationship between fluid-induced hyperchloremia and development of AKI is not yet determined. A recent study demonstrated significant hyperchloremia in dogs with hospital-acquired AKI.16 The most unbalanced isotonic crystalloid is 0.9% sodium chloride because of its high chloride concentration. Plasma-Lyte 148, lactated Ringer’s solution, and Normosol-R have chloride concentrations closer to normal patient plasma concentrations and contain buffers.12
Isotonic crystalloids, hypertonic crystalloids, and/or colloids can be used to treat hypovolemia. In patients with normal vascular permeability, after 30 minutes of IV isotonic crystalloid administration, ≈25% of the fluid remains in the intravascular space, and ≈75% has moved to the interstitial space.
Hypertonic crystalloids (eg, 3%, 7.2%-7.5%, 23.4% hypertonic saline) draw fluid from the interstitial and intracellular spaces, expand the intravascular space because of their high effective osmolality (≤8× higher than blood), and may therefore exacerbate dehydration even while restoring intravascular volume. The primary indications for use of hypertonic saline include life-threatening hypovolemia, severe hyponatremia, and suspected intracranial hypertension due to traumatic brain injury.
Hypotonic crystalloids have a low sodium concentration and thus a higher concentration of free water and are preferable for use as maintenance fluids to replace ongoing sensible (eg, urine, feces, sweat) and insensible (eg, unmeasurable loss from the respiratory tract, GI tract) losses.12 Also due to their low sodium concentration, hypotonic fluids are used to treat hypernatremia and may be preferred in patients with fluid intolerance (eg, from heart or kidney disease) because fluid redistributes more to the intracellular space and less to the intravascular space, decreasing the risk for an increase in hydrostatic pressure.12 Although isotonic crystalloids may be preferred to treat dehydration and/or hypovolemia and hypotonic crystalloids preferred to meet daily maintenance requirements, most patients are managed with isotonic crystalloids alone.12
Hypotonic fluids are not effective as replacement fluids to restore intravascular or interstitial deficits and should not be used to treat dehydration or hypovolemia.17 Infusion of large amounts of hypotonic fluids may cause rapid shifts in sodium concentrations and result in life-threatening cerebral edema.
Writing the Fluid Prescription
The fluid prescription plan is dynamic. The veterinary team (including the clinician, veterinary technicians, and veterinary assistants) should monitor the patient to ensure response to therapy and identify complications. Alterations to the fluid plan are common and should be made based on patient response.
Implementing the Fluid Prescription Plan
Treatment for Hypovolemia
Untreated hypovolemia is life-threatening and may lead to rapid deterioration and death. Hypovolemia may be present with or without dehydration and should be identified based on physical examination findings. Hypovolemic patients should be resuscitated with IV fluids. If hypovolemia is present (with or without dehydration), a large bore peripheral catheter should be placed when possible. If peripheral access cannot be obtained, a central vein (eg, jugular vein) or the intraosseous route can be used.17 Oral, subcutaneous, and intraperitoneal routes should not be used, as these routes rely on perfusion and absorption, which occur too slowly to be effective for treatment of hypovolemia.18
Clinical Skills You’ll Want to Keep
Get this guide in a free downloadable resource, along with guides to 5 more cornerstone skills you'll want to have in your back pocket. From choosing the correct fluid type to performing a neurological examination, Practical Guidance for New Veterinarians is your key to starting practice with confidence.
Isotonic crystalloids should be administered at a fraction of the shock dose of fluids, with the shock dose representing the total blood volume (dogs, 80-90 mL/kg; cats, 50-60 mL/kg).17 Clinical signs of hypovolemia occur when 20% to 25% of blood volume is lost. Reasonable resuscitation is ≈20% to 25% of the total blood volume (dogs, ≈20-25 mL/kg over 15-20 minutes; cats, ≈10-15 mL/kg over 15-20 minutes).17 Fluids should be administered rapidly via high-pressure infusion bags, fluid infusion pumps, syringe pumps, syringes, or manual squeezing of the fluid bag (based on total volume administered and available resources). Concurrent heat support should be provided to hypothermic cats, as cats are most often hypothermic when in shock, and blood vessels may not constrict appropriately when cold. Although this is not a classic finding for dogs in shock, heat support should also be provided to hypothermic dogs. A fluid bolus should not be administered if there is no clinical evidence of shock.
The patient should be re-evaluated after the fluid bolus is administered. If there is a positive response (eg, normotension, lower heart rate, lower lactate, improved mucous membrane color and capillary refill time), the patient should be closely monitored, as an intervention plan may be needed.19 If there is a partial or absent response, the fluid bolus may be repeated up to 3 or 4 times. Diagnostic testing (eg, packed cell volume, total solids, glucose, lactate, point-of-care ultrasound) can be repeated as necessary in patients unresponsive to fluid therapy. Vasopressor therapy can be performed if indicated.20
Hypertonic crystalloids may also be considered in patients with hypovolemia. Hypertonic saline (dogs, 4-6 mL/kg over 10-15 minutes; cats, 1-4 mL/kg over 10-15 minutes) can be administered, ideally in nondehydrated patients with normal sodium concentrations.17 Hypertonic crystalloids can also be used in hypovolemic patients that are also dehydrated, but isotonic crystalloids should be provided concurrently to replace fluid moved from the interstitial space by the hypertonic crystalloid. In addition, hypertonic saline can improve cardiac contractility and rheology and is the fluid of choice for resuscitating patients with suspected cerebral edema. Use of natural and/or synthetic colloids to treat hypovolemia is not described in this article.21,22
Bleeding patients with signs of hypovolemia may require resuscitation with blood products.17 Hypovolemic patients unresponsive to fluid therapy may require inotropes or vasopressors (eg, dobutamine, norepinephrine, vasopressin).18
Many clinically ill patients that require fluid therapy are not hypovolemic and do not require treatment for hypovolemia.
Treatment for Dehydration
If the patient is dehydrated, an intentional rehydration plan can be initiated and the fluid therapy plan calculated based on the estimated amount of fluid lost (ie, fluid deficit): patient’s fluid deficit (L) = body weight (kg) × estimated dehydration % (Table 3).
Table 3: Estimating Dehydration Percentage
aDeath is imminent.
The fluid deficit should be replaced over 4 to 24 hours (average, 12 hours), depending on the individualized patient plan. Longer rehydration times are needed in patients with cardiovascular compromise and/or increased risk for fluid overload. The authors prefer to rehydrate cats over 12 to 24 hours because cats have a higher incidence of occult heart disease.23
Patients should be re-evaluated every 4 hours (or more often if specific concerns exist) and at the end of the rehydration period for resolution of dehydration. Weight gain should be equivalent to the fluid deficit (1 mL = 1 g) but does not always occur if ongoing losses are present.24
Patients with no evidence of hypovolemia or dehydration (eg, obtunded dog [ie, unable to eat or drink] with multiple seizures) may require hospitalization. When there is no evidence of hypovolemia or dehydration, identifying the fluid location and administering isotonic crystalloids can be skipped, and a maintenance fluid plan should be calculated to provide ongoing maintenance fluid needs.
Maintenance Requirements
Dogs and cats have an ongoing fluid requirement for daily cellular and tissue maintenance that should be provided to patients unable or unwilling to eat and drink normally. Although a range of formulas are available to calculate maintenance fluid needs,25 clinicians should use a formula with which they have a high level of comfort to ensure consistency. Based on results of a survey, the most common veterinary maintenance IV fluid rate is 60 mL/kg every 24 hours in cats and dogs25; however, calculations using body surface area may also be used:
(30 × body weight in kg) + 70 (for patients 2-50 kg)
70 × (body weight in kg)0.75
Isotonic or hypotonic crystalloids can provide maintenance fluid needs in dogs and cats.
Diuresis
Fluids may be administered in multiples of maintenance (eg, any rate >45-60 mL/kg every 24 hours [eg, 120 mL/kg or 180 mL/kg every 24 hours]) to provide diuresis, which is only effective for toxins (eg, bromides, amphetamines, phenobarbital) that can be forcibly excreted through the kidneys.26
Forced diuresis is no longer recommended for treatment of azotemia, as these patients should be resuscitated (if required) and rehydrated (often required). Fluids should be provided at maintenance rates until renal or clinical recovery occurs in order to prevent fluid intolerance (ie, fluid overload; diminished capacity to accept additional IV fluids without adverse reaction), which is common in azotemic patients treated with diuresis and may worsen organ function.11
Replacing Ongoing Sensible Losses
Ongoing fluid losses should be replaced when significant losses (eg, irretractable vomiting or diarrhea, polyuria, fluid losses from surgical drains or wounds) occur. Ongoing losses may be objectively measured (eg, urine measured via indwelling urinary catheter) or estimated (eg, for diarrhea). The ongoing loss volume is typically replaced using isotonic crystalloids over 2 to 8 hours, depending on the volume of fluid lost and patient tolerance of fluid replacement.
Monitoring Fluid Therapy
As with all drugs, the fluid therapy plan should be intentional and patients monitored for adverse effects. Common adverse effects include fluid intolerance (especially in patients with underlying heart disease or poor kidney function; see Clinical Signs That May Indicate Fluid Intolerance), interstitial edema (patients with hypoalbuminemia treated exclusively with large volumes of crystalloids), dilution coagulopathy (from excessive administration of crystalloids), or electrolyte and acid–base imbalances.
Clinical Signs That May Indicate Fluid Intolerance
Increased respiratory rate and effort
New cavitary effusion and/or peripheral edema
Excessive weight gain
Hypertension
Chemosis
Case Example
Gracie, a 3-year-old 40-lb (18-kg) spayed Australian shepherd, was presented for anorexia, vomiting, and diarrhea of ≈72-hours’ duration.
On physical examination, mucous membranes were dry, and there was slight skin tenting. Gracie was estimated to be 5% dehydrated. There was no evidence of hypovolemia. Based on physical examination results and initial diagnostic testing, she was hospitalized for supportive care.
An isotonic crystalloid was selected for treatment. The fluid deficit was calculated as: fluid deficit (L) = 18 kg × 5% (0.05) = 0.9 L or 900 mL. In the absence of underlying heart disease or concern for volume overload, the fluid deficit was replaced over 12 hours (75 mL/hour).
The maintenance rate was calculated as: 60 mL/kg × 18 kg = 1,080 mL every 24 hours (45 mL/hour). The final fluid rate was thus: 75 mL/hour + 45 mL/hour = 120 mL/hour for the first 12 hours.
Gracie was evaluated after 12 hours and determined to be well hydrated. The fluid plan was continued at the maintenance rate of 45 mL/hour until she started to show interest in eating and drinking.