Interpreting Small Animal Thoracic Radiographs
Clifford R. Berry, DVM, DACVR, University of Florida

Radiography provides a rapid, noninvasive mechanism for evaluating structures within and surrounding the thorax. Because the changes seen on thoracic radiographs are often indicative of systemic disease (and may be nonspecific), the clinician needs to keep the patient, signalment, physical examination, and other laboratory findings in mind when prioritizing the differential diagnoses.
Considerations
Interpretation of thoracic radiographs can be challenging because most disease processes often involve several areas of the thorax. Thoracic radiographs may be followed by a thoracic computed tomographic study to better characterize or understand the thoracic roentgen abnormalities seen.
High-quality, 3-view thoracic films that are correctly positioned should be the starting point for all practitioners. For best results, the practitioner should be actively involved in processing the images to ensure correct anatomical positioning and exposure (Figure 1). Whenever possible, more than 1 person should review films for abnormalities and roentgen changes.
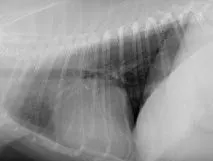
Expiratory (A) and inspiratory (B) right lateral radiographs from a 7-year-old neutered male poodle. Because the act of respiration changes the thoracic appearance, inspiratory films should be attempted to distinguish artifacts from true lung pathology.
Interpretation Paradigm
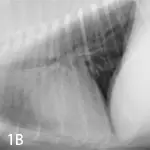
Thoracic radiographs should always be evaluated in the exact same position and correct orientation (ie, left lateral, ventrodorsal or dorsoventral, and right lateral) (Figure 2).



Right lateral (A), left lateral (B), and ventrodorsal (C) thoracic radiographs from a 7-year-old mixed breed neutered male dog. Right lateral (D) and ventrodorsal (E) images from a 4-year-old neutered male domestic shorthair cat. In both cases, the radiographs were deemed normal.
Next, the images should be evaluated using a systematic checklist of thoracic structures. The thorax can be divided into the following 4 compartments:
Extrathoracic structures
Pleural space
Pulmonary parenchyma
Mediastinum
When reviewing films, the clinician should think in terms of radiographic opacity and use the standard roentgen sign approach. Radiographic opacities allow the interpreter to distinguish metal (white), mineral, soft tissue, fat, and air (black).
Each anatomic structure will have specific radiographic attributes that include normal size, shape, opacity, margination (contour), position (location), and number. If a structure appears “abnormal,” the abnormality should be categorized according to the roentgen sign approach because more than 1 change may be present, depending on the disease process.
See Reporting Technique for Thoracic Abnormalities for a form you can use in your clinic to document abnormalities and identify potential differentials.
Author Insight
Most disease processes are multicompartmental in nature (ie, mitral value endocardiosis with cardiogenic pulmonary edema involves the heart within the middle part of the mediastinum and pulmonary parenchyma).
Step by Step: Interpretation of Small Animal Radiographs
Step 1: Extrathoracic Structures
The extrathoracic structures are important and can provide clues as to why a dog or cat is dyspneic or unable to take a deep inspiratory breath, or has secondary features of a primary disease.
Starting in the caudoventral aspect of the radiograph (laterals), structures should be evaluated in the following order:
Sternebrae and costal cartilages
Thoracic limb
Cervical spine
Thoracic spine
Diaphragmatic crura
Diaphragmatic cupola
Cranial abdominal structures
Moving on to the ventrodorsal radiographs, evaluation should start on the caudal right side and proceed in the following order:
Right costophrenic angle
Right-sided ribs and thoracic wall
Right thoracic limb
Cervical and thoracic spine
Left thoracic limb
Left-sided ribs and thoracic wall
Left costophrenic angle
Left diaphragmatic crus
Cupola
Right diaphragmatic crus
Visible cranial abdominal structures
A dog or cat with severe ascites or large cranial abdominal mass will have expiratory radiographs, and no matter what strategy is taken, the radiographs will remain expiratory in nature until the primary abdominal abnormality is addressed.
Step 2: Pleural Space
The pleural space should not be seen on thoracic images from normal animals. A very small amount of fluid, normally present between the visceral and parietal pleura, is imperceptible on thoracic radiographs; however, the pleural fissure lines or interlobar fissures may still be seen within very specific locations (Figure 3).
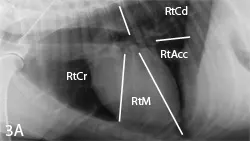

Right lateral (A) and ventrodorsal (B) radiographs from the same dog shown in Figure 2 with the expected locations of the interlobar fissures noted.
Three questions should be asked about the pleural space:
Is there fluid or air within the pleural space?
Are there abdominal organs or pleural mass lesions noted within the pleural space?
Is there an extrapleural sign?
Fluid and air will cause retraction of visceral pleural surface of the lung lobes away from the parietal pleural surface lining the inside of the thoracic wall. If a pleural effusion is present, the fluid will be soft tissue opaque, whereas the adjacent lung will still be radiolucent. This is true unless the lung lobe has disease that will result in a pulmonary soft tissue opacity or atelectasis. If a pneumothorax is present, the area of displacement between the visceral and parietal pleura will be radiolucent without pulmonary vessels or airways; a sharply demarcated lung lobe margin that is soft tissue opaque will also be seen.
If there is an extrapleural sign, a mass lesion (eg, fractured rib, rib tumor) is pushing the parietal pleura into the pleural space (Figure 4). An anatomic variant that routinely results in an extrapleural sign is the costochondral junction of chondrodystrophic dogs, such as the basset hound or the dachshund.

Extrapleural sign (arrow) in a 10-year old basset hound, secondary to the enlarged costochondral junctions and medial deviation of the costal cartilages
Author Insight
An exudative effusion is the most common cause of a unilateral pleural effusion in a dog or cat. The differentials for an exudative effusion include pyothorax, chylothorax, hemothorax, or a neoplastic effusion. Chronic pleural effusions are usually secondary to chylothorax, chronic diaphragmatic ruptures, pyothorax, and neoplastic effusions (eg, rib tumors).
Step 3: Pulmonary Parenchyma
The pulmonary parenchyma is probably the hardest and most frustrating area of veterinary radiology to interpret—or explain. Reasons are many, but a simplified approach can help the clinician arrive at the correct differential list without a tremendous amount of frustration or anxiety.
The first step is to determine whether the pulmonary parenchymal opacity is normal or abnormal. If abnormal, an effort should be made to ensure that this is not an artifact secondary to improper exposure or other technical factors. If the pulmonary opacity is abnormal, then it should be classified as increased or decreased. Based on this categorization, 1 of 2 different interpretive paradigms will apply (see Decreased & Increased Opacity).
DECREASED OPACITY
Generalized Causes
Addison’s disease
Decreased central blood volume
Hyperinflation
Hypovolemia
Pulmonary thromboembolism
Tetralogy of Fallot
Focal/Multifocal Causes
Bronchoeictasis
Bulla/blebs
Cavitated lesion (abscess, tumor, parasites)
Emphysema
Pneumatocoele/hematocoele
Pulmonary thomboembolism
INCREASED OPACITY
Pathology should be anatomically localized by region of thorax & specific lung lobe involved.
Alveolar Pattern (A)
Uniform soft-tissue gray opacity
Lobar sign
Border effacement of heart or diaphragm
Presence of air bronchograms
Bronchial (B)
Usually generalized
Presence of rings and lines
Be sure to evaluate the periphery
Central airways are always prominent
Peripheral thickened airway walls
Vascular Pattern (C)
Enlargement of pulmonary arteries, veins, or both
Intersitial Pattern (D and E)
Structured interstitial (pulmonary nodules; miliary pulmonary pattern)
Unstructured interstitial (backdoor diagnosis in that all other patterns have been ruled out; it is never mild)
Use of the terms infiltrate, consolidation, and bronchointerstitial should be avoided. Each implies nothing more than increased opacity and is not useful when formulating a differential list.
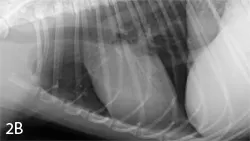
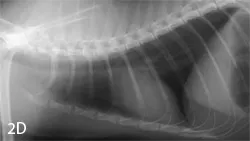
With increased opacity, many diseases will present with a mixed pulmonary pattern, so the dominant pattern should be identified to formulate an appropriate differential list (Figure 5). More important, the anatomic distribution will drive the prioritization process for differentials. For example, cranioventral typically equates with infectious disease (bacterial pneumonia), whereas caudodorsal typically equates with edema (cardiogenic or noncardiogenic).
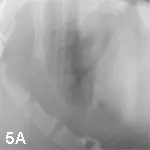
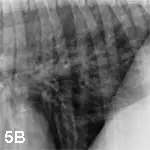
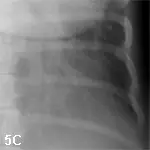

Lateral radiographs from various dogs with increased lung opacity; ventral alveolar pulmonary pattern (A), generalized bronchial pulmonary pattern (B), vascular pulmonary pattern in a dog with a left-to-right shunting patent ductus arteriosus (C), structured interstitial pulmonary pattern in a dog with pulmonary nodules secondary to renal carcinoma metastatic disease (D), and an unstructured interstitial pulmonary pattern (E)
Author Insight
Most causes of an interstitial pulmonary pattern can also cause an alveolar pulmonary pattern, with the only difference being the degree of severity.
Step 4: Mediastinum
The mediastinum can be divided into cranial, middle, and caudal parts. Each area is then divided into dorsal and ventral halves.
Cranial
Within the cranial mediastinum, radiographs should be evaluated for the following changes:
Presence or absence of fluid, air, or mass
Tracheal luminal changes or deviation (hypoplasia or collapse, mass/nodule)
Esophageal abnormalities (foreign body, abnormal distension with ventral deviation of the trachea, mass lesions (Figure 6)
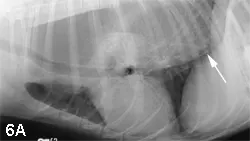

Right lateral (A) and ventrodorsal (B) images from a dog with generalized megaesophagus secondary to myasthenia gravis. Note the ventral deviation of the trachea and heart in the cranial and middle mediastinum. In addition, the dorsal, ventral, and lateral borders of the caudal thoracic radiograph converge to the esophageal hiatus in the central, dorsal third of the diaphragm (arrows).
Depending on the abnormality, a correlative change will be present. The clinician should be on the lookout for cranial mediastinal widening (ventrodorsal film), dorsal or ventral deviation of the trachea (lateral film), displacement of the cranial lung lobes caudally, and abnormal opacities or distension of the esophagus.
Middle
Within the middle mediastinum, the most obvious structure is the cardiac silhouette. Initially, microcardia and cardiomegaly should be noted. In a dog, specific right- or left-side cardiomegaly or cardiac chamber enlargement can be documented; this does not hold true in the cat. Typically, neither the esophagus nor tracheobronchial lymph nodes are visualized in thoracic radiographs from the small animal patient. Enlargement of the tracheobronchial lymph nodes will result in deviation of the right and left cranial bronchi laterally away from the principle bronchial bifurcation, also known as the carina. The carina will be displaced ventrally by enlargement of the central tracheobronchial lymph node, whereas left atrial enlargement will result in dorsal elevation of the carina (Figure 7).

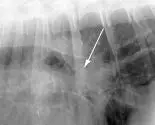
FIGURE 7 Right lateral radiograph from a dog with left atrial enlargement (A). Note the dorsal deviation of the carina secondary to severe left atrial enlargement (arrow). In a radiograph obtained from a dog with enlargement of the central tracheobronchial lymph node (B), ventral deviation of the carina can be seen (arrow).
Caudal
Within the caudal mediastinum, the most common abnormality is esophageal dilation. With a generalized megaesophagus, 2 soft tissue opaque stripes can be seen dorsally and ventrally that converge on the esophageal hiatus of the central diaphragm.
Conclusion
Using a systematic approach to review all aspects of thoracic radiographs will provide the framework for proper evaluation and prevent reader bias, incomplete evaluation, inaccurate interpretation, or overlooked key roentgen abnormalities.