Keratomalacia in the Dog and Cat
Sponsored by Veterinary Products Laboratories
Keratomalacia (“melting cornea”) is a true ocular emergency of dogs and cats. Enzymatic destruction of the corneal stroma, i.e. collagen fibers, and extracellular matrix by protease and collagenase enzymes produces a gray gelatinous corneal appearance. There are multiple sources of the destructive enzymes including bacteria and inflammatory cells. The corneal surface becomes irregular and elevated, producing the characteristic melting appearance and will stain with fluorescein. This ulceration often leads to corneal rupture. Irritation of the axons of the trigeminal nerve initiates an axonal reflex and dilation of vessels of the iris and ciliary body, producing anterior uveitis with aqueous flare often associated with hypopyon.
Contributing factors leading to keratomalacia include inappropriate use of topical antibiotics and corticosteroids. In cats with a history or clinical signs of feline herpesvirus (FHV), Mycoplasma spp. should be considered causative.
Treatment
Cytology and bacterial cultures are necessary in all cases. Pending results, the following treatment regimen is instituted:
Antibiotics that are effective against Gram-negative rods both topically (q2–4h) and systemically
Protease inhibitor topically (serum preferred, q2–4h)
Atropine 1% topically (q24h)
NSAIDs systemically
Hyaluronate tear replacements (q4h, especially if keratoconjunctivitis sicca (KCS) has been previously present)
Duralactin® (animals <40 lb ½ tablet q12h, 40–80 lb 1 tablet q12h, 81–120 lb 1½ tablets q12h) to inhibit migration and infiltration of neutrophils
Cats: medication for FHV orally.
Owners are to be advised to treat around the clock and allow 5 to 10 minutes between topical medications.
The patient should be more comfortable in 48 hours. Antibiotics may change as dictated by cytology and culture. After 72 hours, with noted improvement, the frequency of topical medication can be reduced. If no improvement is seen or if the condition worsens, the diagnosis should be re-evaluated and treatment adjusted or the patient should be referred to a veterinary ophthalmologist. When fluorescein staining is negative, a topical corticosteroid is added to the current treatment regime to reduce vascularization and edema.
It is intuitive that if Duralactin® decreases migration of neutrophils, then its use would be beneficial in treating this condition. I have been using Duralactin® since the1990s in my therapy for keratomalacia in dogs and cats and my clinical impression is that this regimen results in more rapid response and both clearer corneas and more visual eyes than without its addition. Fewer cases require surgical intervention.
Case Histories

A 16-year-old domestic shorthaired cat had a 4 to 6 week history of upper respiratory infection and bilateral ocular disease that failed to respond to various oral and topical antibiotics. The cat was initially treated as outlined above. Following identification of Mycoplasma spp., the oral antibiotic was changed to azithromycin. The image on the right is the same eye 34 days later. Topical corticosteroids were then added. Oral medication was also instituted for presumed FHV infection.
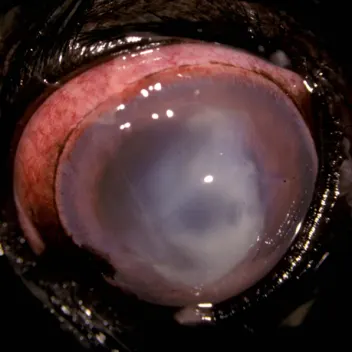
A 5- year-old Shih Tsu had a history of recurring superficial ulcers of the left eye with a normal Schirmer’s tear test. Seven days prior to obtaining the first image, the dog developed a superficial ulcer and was treated with tobramycin, 1% atropine, tear replacements, cyclosporine, and an oral NSAID. The second image is the affected eye 7 days later. Keratomalacia is present with a severe anterior uveitis and hypopyon. The treatment regimen including Duralactin and topical corticosteroids as outlined earlier was begun, with antibiotics changed to topical ofloxacin and oral clindamycin. Clinical signs improved in 4 days and Capnocytophaga spp. was cultured. After 42 days, only mild corneal scarring and vascularization remained.