Neonatal Resuscitation
Amanda A. Cavanagh, DVM, DACVECC, Colorado State University

Figure 1 A neonate is dried and warmed with a clean, dry towel. Tactile stimulation over the umbilicus and genitals helps stimulate respiration. Photo courtesy of Cory Woliver, DVM, Colorado State University College of Veterinary Medicine and Biomedical Sciences
Dystocia and cesarean delivery can result in fetal depression, and neonates may require resuscitation. Physical examination and calculation of viability scores immediately following birth can help ensure prompt and appropriate treatment of neonates and decrease early mortality. A well-trained team familiar with the practice's delivery and resuscitation protocol is essential for a successful outcome. Ideally, each neonate is assigned a dedicated caregiver during delivery, and each caregiver should have a resuscitation plan and all the necessary equipment available.
The most common causes of fetal and neonatal depression are hypoxia and the effects of anesthetics administered to the bitch during cesarean delivery.1 In neonates, hypoxia can cause bradycardia, weak respiratory drive, and flaccid muscle tone.1 Neonates are unable to regulate body temperature because shivering and vasoconstrictive reflexes have not yet developed. Hypothermia often results in bradycardia, tissue hypoxia, metabolic acidosis, ileus, decreased immunity, and slowed metabolism.1-3 Fifty percent of all neonatal deaths occur within 3 days of birth because of hypoxia, hypothermia, and malnutrition.2
Sample Delivery & Resuscitation Plan for Neonates
Clear face and mouth
Use a towel to dry and warm
Assign neonatal viability score. If the score is 0 to 6, begin resuscitation:
Suction nose and mouth
Administer naloxone, if needed
Deliver oxygen and stimulate respiration
Begin compressions and ventilation if bradycardic
Administer epinephrine, if needed
Administer dextrose, if needed
Sever cord and apply tincture of iodine
Provide heat support
Each team member assigned to a neonate should have a resuscitation plan, and his or her resuscitation supplies, including equipment for temperature control and respiratory support as well as catheters for venous access, should be organized before delivery.
Essential Supplies for Neonatal Resuscitation1-3
Warming supplies
Dry towels
Heated incubators with 55% to 65% humidity
Forced-air warming units
Oxygen
Supplemental sources
Small masks
Endotracheal intubation
IV catheters (12- to 16-gauge) can be used as endotracheal tubes in small neonates and kittens
Uncuffed endotracheal tubes (sizes 1-2) can be used in larger neonates
Suctioning
Bulb syringes
DeLee-style aspirator
Venous access
IV catheters (25-gauge)
Spinal needles for intraosseous catheterization
Umbilical care
Small hemostats
Nonabsorbable suture
Sharp, clean scissors
2% tincture of iodine
Monitoring
Rectal thermometer
Pediatric stethoscope
Team members also should be familiar with the medications commonly used in resuscitation, and these drugs should be readily available.
Essential Medications for Neonatal Resuscitation1
Naloxone(0.4 mg/mL)
Dose: 1-2 drops sublingually or 0.1 mL IV
Purpose: To reverse opioid-induced depression
50% dextrose solution
Dose: 1 mL/kg IV diluted 1:4 in warm saline
Purpose: To treat hypoglycemia
Doxapram
Dose: 0.1 mL IV
Purpose: To centrally stimulate respiration; use is controversial
Epinephrine
Dose: 0.1 mg/kg IV of a 1:10 000 solution
Purpose: To restore spontaneous blood circulation
Catheterization in Neonates
IV catheterization is most easily accomplished using the jugular vein.9
Drugs can be administered via the umbilical vein, but the umbilical vein should not be used for catheterization because of its close proximity to the liver. Blood does not circulate through the umbilical vein, so drugs must be diluted into a larger volume of fluid before administration to ensure the drug is transported from the umbilical vein into systemic circulation. The umbilical vein may not be patent if thrombosis has occurred.4,9
Intraosseous catheters can be placed in the femur via the trochanteric fossa, wing of the ileum, tibial tuberosity, or proximal humerus.10
Physical Examination & Treatment
Fetal membranes and fluids should be cleared from each neonate's face immediately after birth. A neonate can often spontaneously clear its airway by vocalizing, but if the neonate fails to vocalize, the nose and mouth should be gently suctioned with a bulb syringe.1
Swinging should never be used to clear a puppy's airway because the practice is dangerous and unnecessary. Swinging puts the neonate at high risk for aspirating stomach contents, developing pneumonia or cerebral hemorrhage secondary to the force of the swinging, and sustaining trauma should the caregiver drop the puppy.1
Each neonate should be immediately dried and warmed via vigorous rubbing with a dry towel. (See Figure 1, top of page.) Drying helps prevent hypothermia, and tactile stimulation, particularly in the genital and umbilical regions, helps stimulate respiration.1 If the bitch received opioids during parturition, naloxone (1 drop sublingually q30min as needed to maintain opioid reversal) should be administered to the neonate as soon as signs of cardiopulmonary depression are observed.
Healthy neonates vocalize and become active during examination; have a strong, immediate suckle reflex; and orient to the bitch using tactile and auditory stimuli.4 Basic physical parameters should be obtained for each neonate and the findings compared with established normal values. (See Table 1.)
Table 1: Normal Physical Examination Parameters in a Neonate Immediately Postpartum
A neonatal viability scoring system can be used to evaluate each neonate's status at birth.5 (See Table 2.) A score of 0 to 3 indicates weak viability and a 4 to 6 score suggests moderate viability. Neonates with scores of 0 to 6 need immediate resuscitation. Neonates with a 7 to 10 score have normal viability and should be monitored closely to ensure continued stability, normal temperature, and normal suckling to receive colostrum.5
Table 2: Neonatal Viability Scoring System5
Respiration
Apnea, weak respiratory effort, bradycardia, failure to vocalize, and lack of vigorous movements indicate the need for resuscitation.
If the neonate fails to draw a breath within 30 seconds or has a slow, irregular respiratory pattern, a tight-fitting mask can be used to deliver 100% O2 and a positive pressure breath at 20 to 30 cm O2 for 3 seconds.1,6 Intubation may be necessary to facilitate adequate lung expansion and continued ventilation at 30 breaths per minute.1
Respiration can be stimulated by placing a 25-gauge needle in the Renzhong or Jen Chung acupuncture point in the nasal philtrum and rotating the needle clockwise against the underlying bone.1 (See Figure 2.)
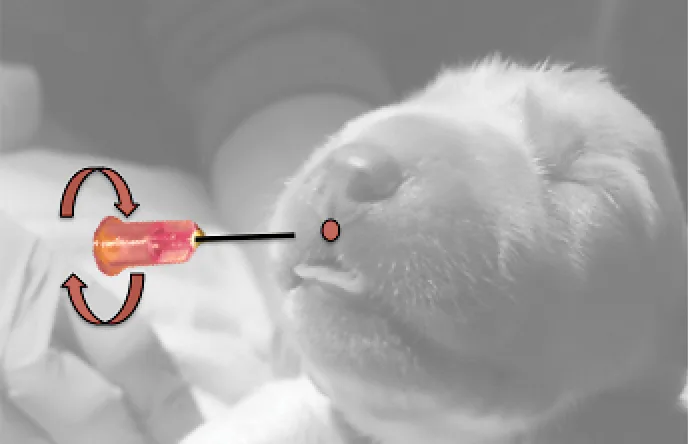
The Renzhong or Jen Chung acupuncture point may stimulate respiration in an apneic neonate. This technique is accomplished using a 25-gauge needle placed into the nasal philtrum and rotated clockwise once the needle contacts underlying maxillary bone. Photos courtesy of Amanda A. Cavanagh, DVM, DACVECC
Doxapram is a central respiratory stimulant that is ineffective in a hypoxic cerebral environment. Use of this drug is controversial.1,6
Heart Rate
Because bradycardia and asystole occur secondary to myocardial hypoxia, heart rate often normalizes following respiratory resuscitation.4,7 If bradycardia persists, thoracic compressions and continued ventilation are indicated. If compressions fail to achieve an adequate heart rate and pulse, epinephrine should be administered intravenously.
Atropine has minimal to no effect on heart rate in puppies and kittens younger than 2 weeks and is contraindicated.8 Glycogen stores in neonates are rapidly depleted, and these patients are susceptible to hypoglycemia.1,2 Crying, weakness, seizures, and coma are all signs of hypoglycemia. Dextrose can be administered intraosseously or intravenously to neonates who remain neurologically depressed, even if a blood sample cannot be obtained to confirm hypoglycemia.

A neonate delivered vaginally has cyanosis secondary to an inadequate respiratory drive. The bitch presented with dystocia because of malpresentation of the first puppy.
Defects
Following stabilization, a thorough physical examination should be performed to identify congenital defects and acquired conditions, including infection. The oral cavity, umbilicus, urogenital structures, limbs, and skin should be examined carefully, and cardiothoracic auscultation should be performed to evaluate heart and lung sounds.4
Hypothermia, failure to suckle, diarrhea, dehydration, cyanosis (see Figure 3), and skin sloughing of the extremities (see Figures 4 & 5) are abnormal findings3,6 and should be addressed promptly.

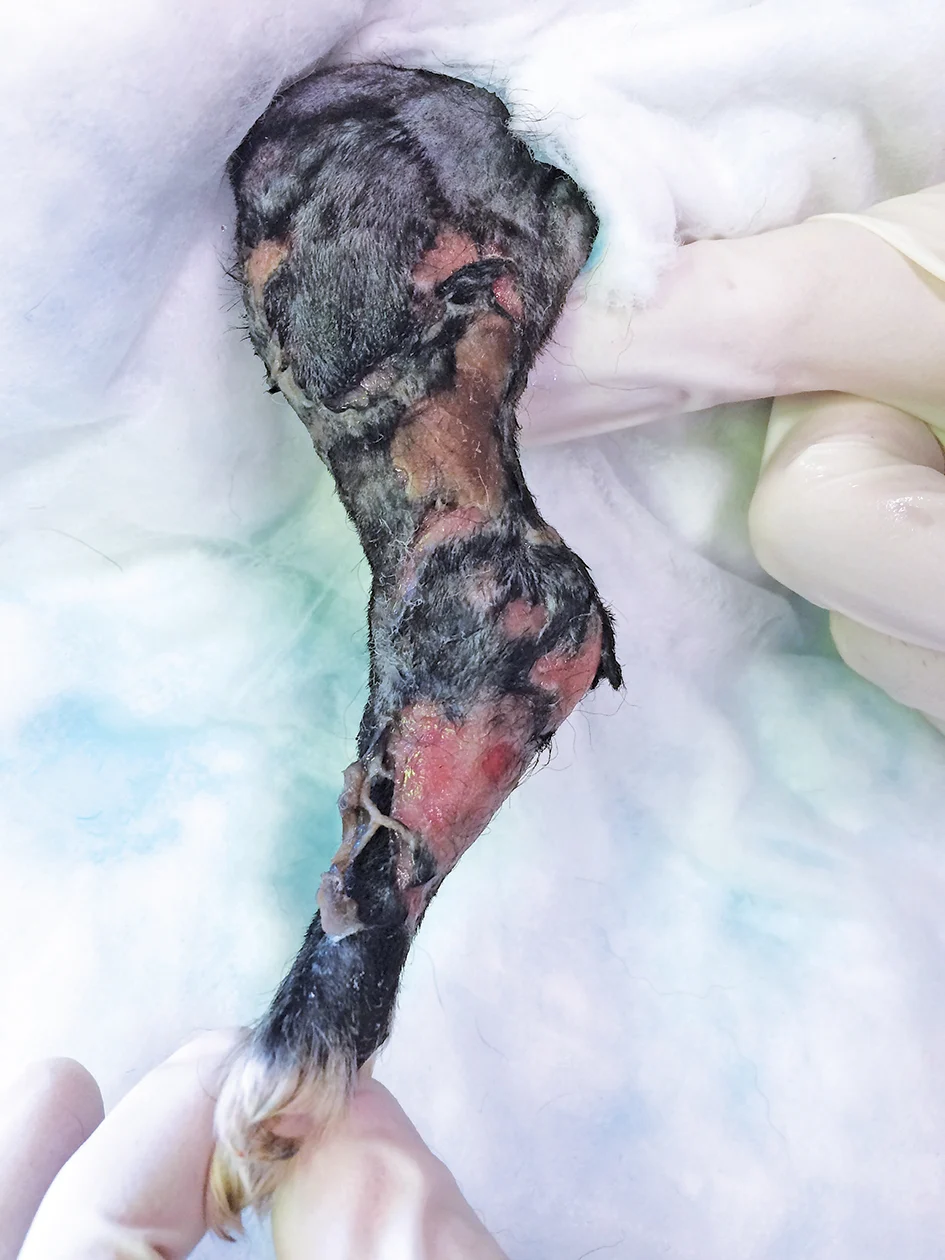
A 4-day-old neonate's skin is sloughing from the hind limb secondary to neonatal septicemia originating from the umbilicus.
Umbilical Cord
The umbilical cord should be ligated with suture 1 cm from the abdominal wall and cut with clean scissors. Application of a 2% tincture of iodine prevents bacterial colonization and ascension into the peritoneal cavity and promotes desiccation of the umbilicus.4
Neonates acquire passive immunity via ingestion of adequate colostrum, which protects them from infectious agents within the first 24 hours postpartum.4 Maternal serum (15 mL/100 g body weight) can be administered via orogastric tube if colostrum is unavailable.6 After 24 hours, IgG cannot be absorbed across the intestinal mucosa and serum must be administered subcutaneously (5 mL/100 g body weight q6h for 3 doses) to impart passive immunity.4,6
Heat Support & Weight
Until neonates are 4 to 6 weeks of age, they should be provided a source of external heat support that maintains an environmental temperature of 86°F to 90°F and humidity of 55% to 65%.3,4,6
Each neonate should be weighed twice daily to identify weight loss or failure to gain weight, which may indicate an inability to obtain adequate nutrition.4 Neonates should gain at least 10% of their body weight per day.4 Low birth weight and failure to gain weight increase risk for early death in neonates.2
Client Communication Points
Hypoxia and opioid-induced cardiopulmonary depression are common causes of neonatal depression following dystocia and cesarean delivery. Resuscitation focuses on adequate oxygenation and ventilation and is essential for decreasing early mortality in affected neonates. Heat support prevents hypothermia and its adverse events on the cardiovascular, GI, and immune systems. Ideally, one skilled caregiver should be present during delivery for each expected neonate, and each caregiver should have a delivery and resuscitation plan in place before the procedure.
This article originally appeared in the June 2017 issue of Veterinary Team Brief.