Pelvic Limb Lameness in a Golden Retriever Puppy
Mary Sarah Bergh, DVM, MS, DACVS, DACVSMR, Midwest Veterinary Specialists, Milwaukee, Wisconsin

Maggie, a 5-month-old female golden retriever, was presented 2 hours after her owner observed an acute onset of right pelvic limb lameness. No causative incident for the lameness had been observed.
Physical Examination
On physical examination, Maggie was bright, alert, and responsive. Vital parameters were within normal limits, aside from an elevated heart rate (140 bpm) presumably due to discomfort. Thoracic auscultation was within normal limits. She was nonweight-bearing on her right pelvic limb, and the stifle joint was visibly swollen with palpable pain. Range of motion in the right stifle was reduced. The remainder of the clinical examination was within normal limits.
Diagnosis
Differential diagnoses for this patient’s stifle swelling, pain, and lameness included fracture, patellar luxation, cranial cruciate ligament injury or avulsion, muscle or tendon strain, osteochondritis dissecans, and septic arthritis. Although there was no known trauma, fracture remained on the differential list, as juvenile bone is soft and the physes are weaker than the adjacent bone and ligaments, which can lead to fractures that can occur with little or no apparent trauma.1-4 Early identification and treatment of physeal fractures are important to minimize the risk for development of significant limb deformities, joint incongruities, and intractable lameness.1-3
Hydromorphone (0.05 mg/kg IV) was administered for analgesia, and lateral and ventrodorsal thoracic radiographs were obtained to evaluate for thoracic trauma. Radiographic findings were within normal limits; however, lateral and craniocaudal radiographs of the right pelvic limb (Figure 1) revealed a Salter-Harris type II fracture of the distal femur with caudal and medial displacement.
Although Maggie’s fracture was not difficult to identify on radiographs, not all physeal fractures are as easily identified. Radiography of the contralateral joint for comparison can help confirm diagnosis.5,6 Radiography can also be repeated 10 to 14 days later to look for signs of physeal damage if the diagnosis remains unclear.5,6
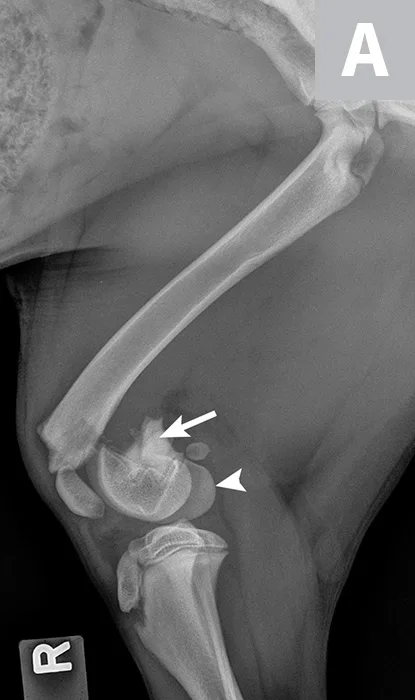

Lateral (A) and craniocaudal (B) radiographs of this patient’s femur. A Salter-Harris type II fracture with caudal and medial displacement is present in the distal femur. The metaphyseal component (A; arrow) and the epiphyseal component (arrowhead) can be noted.
DIAGNOSIS: SALTER-HARRIS TYPE II FRACTURE
TREATMENT AT A GLANCE
A thorough orthopedic examination should be performed on all puppies and kittens presented with acute lameness.
Surgical repair is indicated in most cases to restore limb alignment and provide stability of the fracture.
Gentle tissue handling during surgery is important to preserve blood supply to the tissue.
Smooth pins can be beneficial in the stabilization of physeal fractures.
Stable fixation is critical to allow for early mobilization of the fractured limb.
Physical therapy should be initiated postoperatively.
Implants do not usually need to be removed after the fracture has healed unless they interfere with patient growth or comfort.
Treatment & Long-Term Management
Early surgical repair of physeal fractures is key to restoring limb function and minimizing damage to the fractured physis (see Treatment at a Glance). The basic principles for treatment of physeal fractures are preservation of blood supply, anatomic reduction, and stable fixation. Gentle soft tissue handling during fracture reduction and stabilization is essential to avoid damage to the soft juvenile bone and soft tissue surrounding the fracture site. When applied nearly perpendicular to the physeal surface, smooth pins can allow for continued growth, as the proliferating cartilage can slide along the pins. Implants should be placed so they do not interfere with joint function.
Maggie was managed overnight with analgesia (ie, hydromorphone [0.05 mg/kg IV q4-6h]) and nursing care. The following morning, Maggie was placed under general anesthesia and given a morphine epidural, and surgical fixation of the fracture was performed through a craniolateral approach to the stifle. The distal femoral physis is W-shaped and has inherent stability when reduced; however, additional stabilization is required to provide adequate resistance to the forces applied across the fracture and to allow for the stability needed for healing. Two smooth pins were placed obliquely across the fracture site (Figure 2). The pins should cross proximal to the fracture site to provide maximal repair stability.7
Postoperation, Maggie’s pain was managed with cryotherapy and hydromorphone (0.05 mg/kg IV q4-6h) until she was eating, at which time she was transitioned to carprofen (2.2 mg/kg PO q12h); her comfort level was determined to be good. Additional analgesic options to consider could include gabapentin or codeine if deemed necessary. Physical rehabilitation was initiated the first day postoperation and included massage and range-of-motion exercises of the limb. Exercise restriction and continued physical rehabilitation therapy were advised until radiographic follow-up could be performed 5 weeks postoperation. Early mobilization of the limb is important to encourage mobility, prevent periarticular fibrosis, and, in cases of distal femoral fractures, help prevent the development of quadriceps contracture.8,9


Lateral (A) and craniocaudal (B) radiographs of the femur immediately after open reduction and internal fixation with 2 cross pins. The pins cross proximal to the fracture site, which is important for stability of the repair.
Prognosis & Outcome
At the 5-week postoperative examination, Maggie was fully weight-bearing on her right pelvic limb and the stifle had full and pain-free range of motion. Radiography of the stifle revealed that the fracture was healed, the implants were stable, and the distal femoral physis was closed (Figure 3). A closed distal femoral physis is a common finding after fracture repair, as the germinal cells, which are responsible for physis growth, are frequently irreversibly damaged during the fracture event. Premature physeal closure can result in shortening of the femur, particularly if the animal is young and has large remaining growth potential.2,10 However, a closed distal femoral physis in a dog of Maggie’s age does not usually result in a clinical problem, as dogs are generally able to compensate for mild limb length discrepancies through extension of adjacent joints and compensatory overgrowth of the tibia.2,10
Maggie had uncomplicated healing and an excellent outcome and was allowed to return to normal activity by 8 weeks postoperation. The pins were left in situ. Maggie grew into adulthood and continues to have normal function of her fractured limb.


Lateral (A) and craniocaudal (B) radiographs of the femur 5 weeks after fracture repair. The fracture has healed and the distal femoral physis has closed.
Discussion
Salter-Harris fractures occur through the physes in juvenile animals.4 The Salter-Harris classification scheme categorizes fractures based on a scale of I to V according to anatomic location of the fracture relative to the physis, epiphysis, and metaphysis (Table; see Suggested Reading).4 A Salter-Harris type II fracture, as seen in Maggie, occurs through the physis and extends into the metaphysis4 and is a common fracture pattern seen in the distal femur of puppies.1,8,11 The distal femoral physis closes between 6 and 11 months of age, and bone growth from this physis contributes 75% of the length of the canine femur.2,12
SALTER-HARRIS FRACTURE CLASSIFICATION
*The physis is the growth plate. The cells in this region are responsible for the longitudinal growth of the bone. Radiographically, this region is more lucent than the adjacent bone.
<sup†sup>The metaphysis is the region of bone between the physis and the diaphysis and consists of newly formed bone from the physis.
<sup‡sup>The epiphysis is the region of bone between the physis and the joint space. Fractures through the epiphysis are articular fractures.
Early identification and treatment of physeal fractures is important to maximize patient outcomes (see Take-Home Messages). Orthogonal radiographs of the area of concern should always be obtained and can be compared with radiographs of the contralateral joint. Careful surgical technique is important when repairing physeal fractures, as excessive dissection may damage the blood supply and germinal cell layer in the fracture plane, resulting in early physis closure. Anatomic reduction of the fracture is essential to maintain the potential for longitudinal growth from the physis and restoration of limb alignment.
Prognosis following physeal fractures can be very good. In humans, prognosis worsens as the fracture classification number increases, although this may not be true in animals, as human prognosis does not take into account patient age, remaining growth potential of the patient, and fracture location, all of which can more significantly impact the outcome in veterinary patients.1,2,13 Prognosis is best if the fracture is identified and repaired quickly with anatomic reduction and rigid fixation. Perioperative analgesia and postoperative physical rehabilitation can improve patient comfort and maximize clinical outcomes. If the fracture involves the articular surface, some degree of osteoarthritis can be expected over time but is usually minimal when good surgical technique is used. Maggie’s outcome is similar to most dogs that undergo surgical repair of Salter-Harris type II fractures.2,11 Prognosis may be less favorable in younger patients and in patients with more soft tissue trauma, compromised blood supply to the fracture area, chronic fractures, fractures with marginal or unstable repairs, and/or greater amount of remaining growth potential.2 As in Maggie’s case, the implants can remain in place unless they migrate or cause irritation.2,11
TAKE-HOME MESSAGES
A high index of suspicion for Salter-Harris fracture should be maintained in juvenile animals with acute lameness.
Salter-Harris fractures can occur secondary to minimal trauma because the physis is weaker than the surrounding bone.
Radiography of the affected area should be performed. Radiographs of the injured region should be compared with radiographs of the contralateral side if the physeal appearance is uncertain.
Early surgical repair with good technique is critical to a successful patient outcome.
Physical rehabilitation therapy is an important component that should be implemented to maximize recovery.
Outcome is typically better in animals with less remaining growth potential (ie, >6 months of age).