
Although endocrine tests (eg, luteinizing hormone and progesterone assays) are typically used to monitor the canine female reproductive cycle and help determine readiness to breed,1-3 vaginal cytology is invaluable for evaluation of normal and abnormal cycles and identification of pathology of the lower genitourinary tract. Obtaining quality samples from the correct anatomic site and interpreting cells can be challenging.4,5
Step-by-Step: Performing Vaginal Cytology in Dogs
What You Will Need
Sedation (optional)
Large, clean, disposable otoscope cone and lighted otoscope (may not be needed for small dogs)
Cotton-tipped applicators moistened with saline or distilled/sterile water
Glass microscope slides
Stains (eg, Romanowsky-type stain) for cytology
Light microscope
Immersion oil and coverslip (if slide will be saved)
Step 1: Administer Sedation (Optional)
Provide mild sedation to full anesthesia as needed in dogs in diestrus or anestrus, exhibiting signs of anxiety, or with pathology that may produce pain.
Author Insight
Most dogs in proestrus or estrus are compliant for vaginoscopy.
Step 2: Perform Vaginoscopy (Optional, Depending on Patient Size)
Moisten an otoscope cone with saline or distilled/sterile water (unless there is already abundant discharge) connected to a lighted otoscope, and introduce the cone at the dorsal commissure of the vulva. Advance the cone dorsocranially at a 45-degree angle (avoiding the ventrally located clitoral fossa), until the vagina goes from an upward 45-degree angle to an almost 90-degree angle, and into the anterior vagina.4,6-8
Author Insight
Although vaginal cytology can be performed without an otoscope and attached cone, viewing the vagina through the otoscope may lead to discovery of congenital anomalies (eg, vaginal bands, vagino-vestibular strictures) or neoplasia (eg, transmissible venereal tumors).9,10
Step 3: Collect & Create a Diagnostic Sample
Use a cotton-tipped applicator moistened with saline or distilled/sterile water and inserted through the cone to swab the vaginal mucosal surface to obtain representative cells.6-8 Avoid swabbing the clitoral fossa (which can be painful and only yields cornified cells) and the urethral opening (which can be painful and complicate interpretation of results).4,6-8 Roll the swab onto a glass slide, and allow the sample to air dry prior to staining. View stained slides at lens magnifications of 10×, 40×, or 100× magnification.6-8

Figure courtesy of Bruce E. Eilts, DVM, MS, DACT
Step 4: Interpret Vaginal Epithelial Cell Types
Identify noncornified (ie, parabasal, intermediate) and cornified (ie, superficial, anuclear) cells to determine the patient’s estrous cycle stage.
Author Insight
Following is a representation of the anterior vagina at various stages of the estrous cycle, including expected cell types and a representative hormone profile of estrogen and progesterone for each stage.

Letters correspond with Figures A-G.

Anestrus—relatively few cells are present; a noncornified parabasal cell (black arrow), neutrophil (white arrow), and proteinaceous material are visible. 100× magnification

Early proestrus—noncornified cells (mostly small parabasal [arrow], some intermediate [star]) are present; RBCs (not seen here) may be present in abundance. 10× magnification

Mid-proestrus—noncornified intermediate cells (star) and some cornified cells (superficial and occasional anuclear squamous) (arrow) are present; presence of bacteria is considered normal. 100× magnification
Late proestrus—large number of cornified cells (superficial and squamous) are present; progesterone is 1.32 ng/mL. 10× magnification

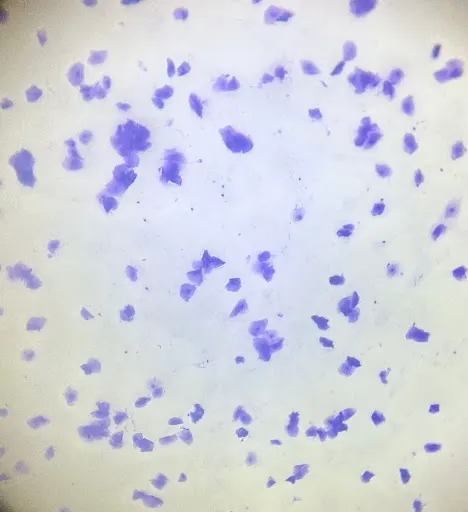
Estrus—large number of 100% cornified cells (anuclear squamous) are present with very little background; progesterone is >11 ng/mL. 100× magnification

Diestrus (day 1)—sharp return back to noncornified cells (black arrow) with neutrophils (white arrow) can be seen. 100× magnification

Mid-diestrus (day 35)—after luteinizing hormone (LH) peak; many noncornified cells (mostly parabasal [arrow], some intermediate [star]) are present. 10× magnification
Progression of Noncornified & Cornified Cells
Noncornified parabasal cells are closer to the basement membrane of the vagina and are present at every reproductive stage but are less commonly seen as dogs progress through the estrous cycle.6,7 Under the influence of estrogen, some parabasal cells divide, enlarge, and develop a higher cytoplasm:nucleus ratio and become intermediate cells.6,7 Continuation of this transformation leads to cornified cells (eg, superficial, anuclear squamous). Superficial cells are larger than intermediate cells, have irregular borders, and have a smaller nucleus than noncornified cells. Anuclear squamous cells are the last cell type formed and appear in abundance later in the estrous cycle. These cells have irregular borders, pale cytoplasm, and a pyknotic or absent central nucleus.6,7 Parabasal cells reappear at the conclusion of estrus (day 1 of diestrus).6,7
Additional Cell Types
Other cells (eg, RBCs, neutrophils) may occupy the vaginal tract in varying amounts at different stages of the estrous cycle.6,7 Estrogen causes migration of RBCs across uterine arteries into the vaginal lumen (ie, diapedesis), resulting in bloody discharge typically seen during proestrus and early estrus. Neutrophils are most commonly seen during early diestrus.6,7 An abundance of neutrophils may be seen along with the return of parabasal cells on day 1 of diestrus. A parabasal cell engulfing a neutrophil may be referred to as a metestrum cell.6,7
Bacteria
Bacteria is normal during any stage but is less commonly seen during estrus because of the high number of cornified anuclear squamous cells. Without clinical signs supportive of infection, the significance of bacteria should be considered with caution.6,7,11,12
Interpreting Cell Types in Vaginal Discharge
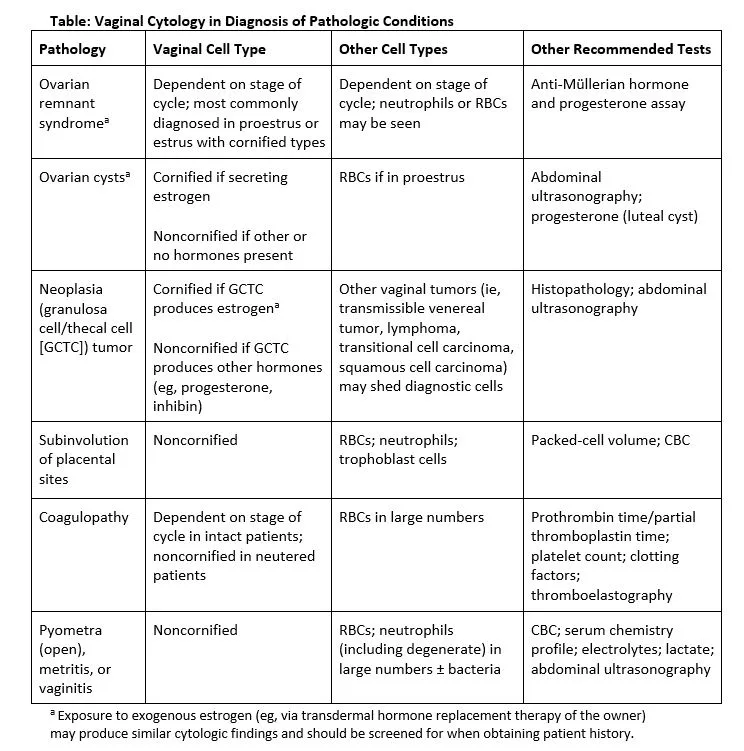
Although vaginal cytology is commonly used to identify estrous cycle stage in normal healthy dogs, it can be used to identify vaginal cell types present in response to pathologic conditions that may cause hyperestrogenism or an influx of neutrophils from inflammation (Table).7,9,13,14
Author Insight
An ovarian cyst secreting estrogen can result in profound cornification of vaginal epithelial cells, similar to during estrus (A, 100× magnification).

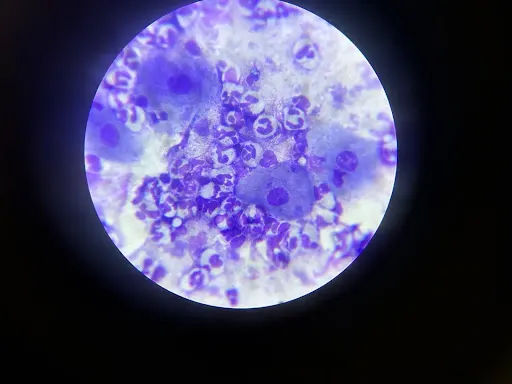
Production of estrogen by Sertoli cell tumors in male dogs can produce similar cornification of the preputial mucosa (B, 10× magnification) because the inner lamina of the prepuce and the vagina are derived from the same embryologic tissue.15 Healthy, intact male dogs should have noncornified preputial cells (C, 100× magnification).

Related: Quiz: Canine Uterine Disorders